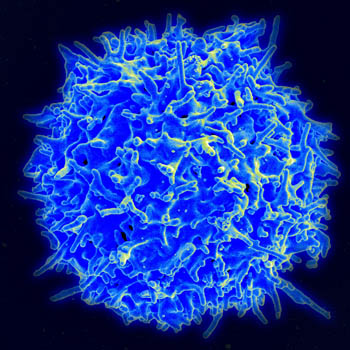
Immunologists at St. Jude Children’s Research Hospital have identified biochemical “switches” that control development of regulatory T cells and offer a novel strategy for treatment of autoimmune diseases and cancer. The research appeared earlier this month in the journal Cell Reports.
The findings mark significant progress in understanding regulatory T cell development and function. The results come amid continuing intense interest in the clinical potential of these immune cells. Regulatory T cells help to maintain and fine-tune immune balance, which is key for preventing autoimmune diseases or enhancing cancer treatment.
“The work defines how regulatory T cells come to act as immune suppressors and knits fragmentary observations into a coherent understanding of the process,” said corresponding author Yongqiang Feng, Ph.D., of the St. Jude Department of Immunology. “This new model offers a stage-specific, drug-targeting approach and practical guidance for future clinical trials.”
Three-step process
The research focused on the Foxp3 protein. Scientists knew Foxp3 expression was essential for transforming precursor immune cells into immune-suppressing regulatory T cells. But knowledge was limited about how Foxp3 expression was precisely controlled.
Working in mouse T cells, researchers identified a three-step biochemical process. Feng compared the steps to starting an engine and keeping it running.
Step 1: Precursor cells receive guidance signals and initiate regulatory T cell development.
Step 2: An epigenetic mechanism called histone acetylation serves as the switch that turns on Foxp3 expression, much as a battery starts an engine. Histone acetylation involves adding a chemical tag to chromatin to promote expression of the Foxp3 gene.
Step 3: Another epigenetic process called DNA demethylation takes over to keep Foxp3 expression going much as fuel keeps an engine running. In this step, a chemical tag is removed from DNA. Surprisingly, once DNA demethylation begins, histone acetylation is no longer necessary, like a battery for a running engine.
Researchers previously reported that vitamin C and the short-chain fatty acid butyrate—made by health-promoting bacteria in the gut—enhanced Foxp3 expression. Now it is clear that they act at different steps in the process.
Clinical potential
“In this study we asked fundamental questions about how exactly regulatory T cells are made,” Feng said. “We think that understanding fundamentals will help people precisely manipulate these cells in the future to treat cancer or autoimmune diseases.”
At each step in regulatory T cell development, the research revealed distinct mechanisms that could be targeted to increase or decrease the number of regulatory T cells to improve human health, he said.
More information:
Jun Li et al, Control of Foxp3 induction and maintenance by sequential histone acetylation and DNA demethylation, Cell Reports (2021). DOI: 10.1016/j.celrep.2021.110124
Provided by
St. Jude Children’s Research Hospital
Citation:
Secrets of regulatory T cell development reveal clinical possibilities (2021, December 29)