Before COVID-19, there was tuberculosis. Twentieth century British physician Thomas McKeown controversially proposed that the sharp declines in infectious disease death rates in the late 1900s were due to improved economic and social conditions – not medical and public health measures like antibiotics and improved sanitation.
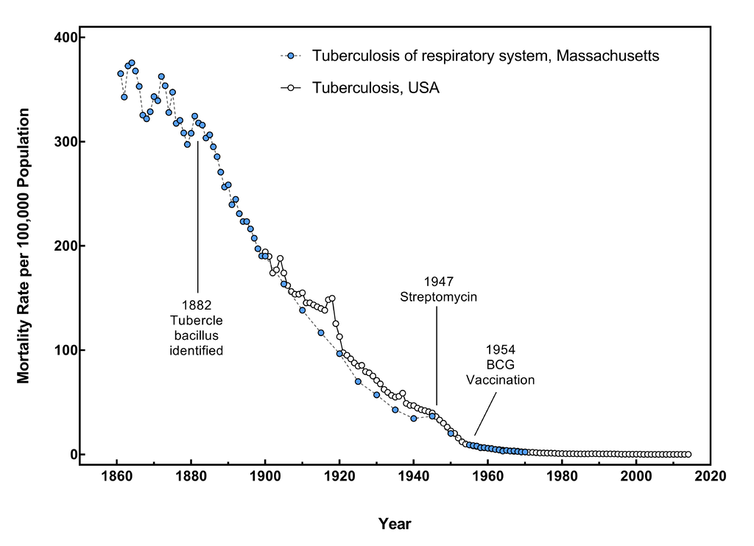
This graph shows the tuberculosis death rate in Massachusetts from 1861-1970 and in the U.S. overall from 1900-2014, using merged data from the U.S. Census Bureau and the Centers for Disease Control and Prevention. While not the same graph that McKeown used, it shows a similar trend that highlights the steep decrease in death rates that occurred before antibiotics and vaccination became available.
Ljstalpers/Wikimedia Commons, CC BY-SA
His theory was later partly discredited. But the central question behind it – whether medical interventions or social factors make the biggest impact on infectious diseases – remains relevant in the current pandemic.
When COVID-19 first arrived in the U.S., the only tool public health officials had to stop its spread was behavior change through lockdowns, social distancing and face masks. With vaccines, the tide seemed to turn. But with new variants, waning immunity and ongoing vaccine hesitancy, the pandemic is still far from over.
So which are more successful at driving down rates of disease and death – social behaviors or medical technologies?
As an infectious disease and social epidemiologist, I have been particularly interested in how new medical technologies affect existing health disparities. I believe that understanding the interplay between behavior and technology will be key to surviving the pandemic and emerging as a stronger society.
Do technologies help or make things worse?
Biomedicine has clearly played a critical role in mitigating COVID-19. Less than a year after discovering the virus that causes COVID-19, researchers were able to develop multiple vaccines that are highly effective in preventing severe infection and transmission from most variants. They’re also likely to reduce the risk of long COVID-19, the ongoing symptoms that can persist for months after initial recovery. COVID-19 vaccines are estimated to have saved almost 140,000 lives in the U.S. in the first five months of 2021.
There has also been remarkable medical progress in other arenas. Even though antivirals are notoriously difficult to manufacture, there are finally options for treating COVID-19. Merck’s molnupiravir cuts hospitalization risks for adults in half, and Pfizer’s paxlovid has 89% efficacy at preventing hospitalization and death. Additional treatments are expected in the coming months.

