The opioid crisis remains a significant public health challenge in the United States. In 2022, over 2.5 million American adults had an opioid use disorder, and opioids accounted for nearly 76% of overdose deaths.
Some patients are fearful of using opioids after surgery due to concerns about dependence and potential side effects, even when appropriately prescribed by a doctor to manage pain. Surgery is often the first time patients receive an opioid prescription, and their widespread use raises concerns about patients becoming long-term users. Leftover pills from a patient’s prescriptions may also be misused.
Researchers like us are working to develop a personalized and comprehensive surgical experience that doesn’t use opioids. Our approach to opioid-free surgery addresses both physical and emotional well-being through effective anesthesia and complementary pain-management techniques.
What is opioid-free anesthesia?
Clinicians have used morphine and other opioids to manage pain for thousands of years. These drugs remain integral to anesthesia.
Most surgical procedures use a strategy called balanced anesthesia, which combines drugs that induce sleep and relax muscles with opioids to control pain. However, using opioids in anesthesia can lead to unwanted side effects, such as serious cardiac and respiratory problems, nausea and vomiting, and digestive issues.
Concerns over these adverse effects and the opioid crisis have fueled the development of opioid-free anesthesia. This approach uses non-opioid drugs to relieve pain before, during and after surgery while minimizing the risk of side effects and dependency. Studies have shown that opioid-free anesthesia can provide similar levels of pain relief to traditional methods using opioids.
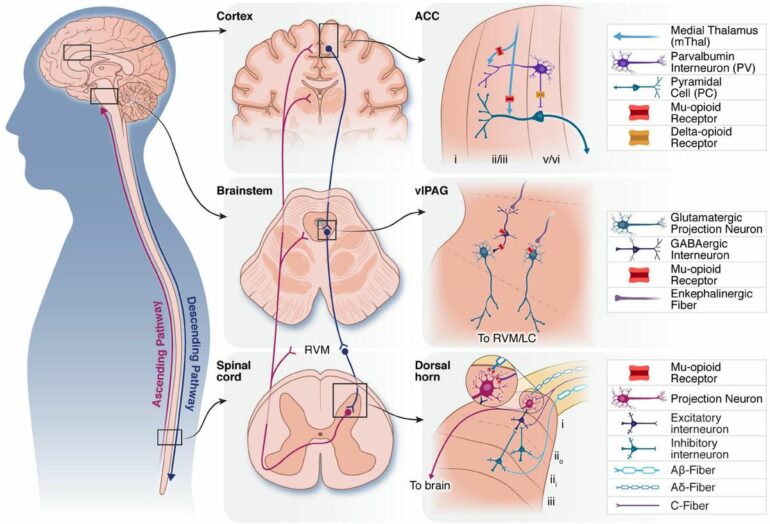
Opioid-free anesthesia is currently based on a multimodal approach. This means treatments are designed to target various pain receptors beyond opioid receptors in the spinal cord. Multimodal analgesia uses a combination of at least two medications or anesthetic techniques, each relieving pain through distinct mechanisms. The aim is to effectively block or modulate pain signals from the brain, spinal cord and the nerves of the body.

Balanced anesthesia combines a number of different drugs to ensure a smooth surgery.
bymuratdeniz/E+ via Getty Images
For instance, nonsteroidal anti-inflammatory drugs, or NSAIDs, such as ibuprofen work by inhibiting COX enzymes that promote inflammation. Acetaminophen, or Tylenol, similarly inhibits COX enzymes. While both acetaminophen and NSAIDs primarily target pain at the surgical site, they can also exert effects at the spinal level after several days of use.
A class of drugs called gabapentinoids, which include gabapentin and pregabalin, target certain proteins to dampen nerve signal transmission. This decreases neuropathic pain by reducing nerve inflammation.
The anesthetic ketamine disrupts pain pathways that…