Among the many challenges that the COVID-19 pandemic presented, disruptions in health care were among the most impactful. The pandemic was large-scale, lasted over two years, and resulted in millions of hospitalizations and 1.2 million deaths in the United States alone. Meanwhile, routine medical services were affected by the pandemic; patients avoided health care visits for fear of contracting the virus; stay-at-home policies left patients without routine care; and there was a limited supply of services.
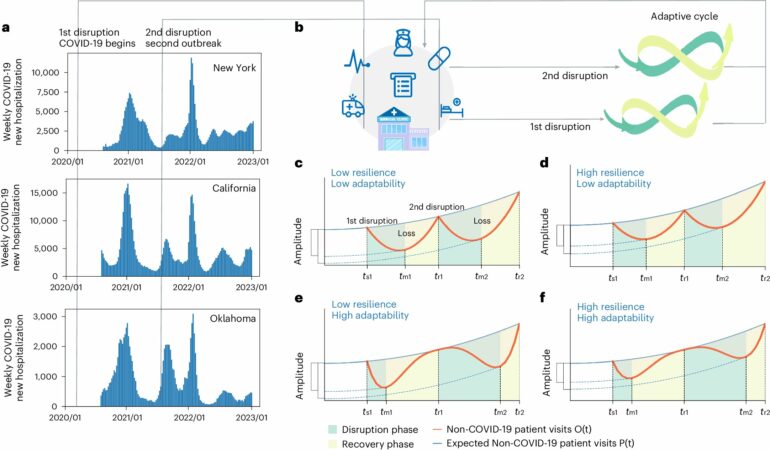
In research recently published in Nature Medicine, Rensselaer Polytechnic Institute’s Jianxi Gao, Ph.D., associate professor of computer science, and his team measured the resilience and adaptability of our health care system to disruptions caused by COVID-19. Resilience is a system’s ability to absorb and recover from disruptions. Adaptability is a system’s ability to learn from previous disturbances where there are recurrent disruptions.
Gao and team analyzed millions of patient records using electronic medical record data and examined 23 essential health care services over a broad range of health needs including chronic disease care and maternal care.
“We found that our health care systems in the United States exhibit substantial adaptability, but only a moderate level of resilience,” said Gao. “Our findings can inform the design of resilient and sustainable health care systems to prepare for future disruptions, whether they are caused by pandemics, climate change, conflicts, or anything else.”
Gao and his team found that the health care system underwent two waves of disruptions. Over 90% of the health care systems performed better during the second disruption, which demonstrates adaptability. However, by the end of 2022, about 77% of health services had yet to fully rebound to normal levels.
In states with high poverty levels and high unemployment, health care systems showed low resilience and adaptability, as determined largely by physician abundance. Additionally, chronic disease care was more resilient and adaptive than maternal care, likely because long-term treatments are more flexible in delivery across settings from home care to primary care to specialty care. Services for heart disease management demonstrated lower resilience and adaptability than conditions such as asthma, COPD, cancer, and diabetes.
Gao and team also found that the pandemic severely affected the health care of Black and Hispanic populations, with harsher disruptions and lower resilience. The disparities may result from socioeconomic inequalities that Black and Hispanic communities face in accessing health care services, particularly during disruptions.
“The good news is that we can learn from this research and make changes to our health care systems for better outcomes,” said Gao. “We can strategically place physicians and focus resources on areas that we’ve determined are vulnerable.”
“Dr. Gao’s framework for quantifying health care system resilience is revealing valuable insights to help ensure routine health care does not suffer during a future prolonged crisis,” said Curt Breneman, Ph.D., dean of Rensselaer’s School of Science. “This research provides policymakers with the tools they need to modify policies to ensure all populations get equitable access to health care, even under extraordinary circumstances.”
Gao was joined in research by Lu Zhong, Ph.D., postdoctoral research associate at Rensselaer; Dimitri Lopez, graduate researcher at Rensselaer; and Sen Pei, Ph.D., assistant professor in the Department of Environmental Health Sciences at Mailman School of Public Health of Columbia University.
More information:
Lu Zhong et al, Healthcare system resilience and adaptability to pandemic disruptions in the United States, Nature Medicine (2024). DOI: 10.1038/s41591-024-03103-6
Provided by
Rensselaer Polytechnic Institute
Citation:
Researchers draw insights from COVID-19 to inform improved health care in times of crisis (2024, July 18)