A new study reveals a staggering disparity in life expectancy between Black Americans and their white counterparts between 1999 and 2020. In an analysis of U.S. data, a Yale-led team of researchers found 1.63 million excess deaths in the Black population compared with white Americans, representing more than 80 million excess years of potential life lost.
The findings drive home the urgency of making health equity a reality and the need for policymakers and health care professionals to address structural racism and health disparities, the researchers say. While some progress toward reducing disparities was achieved in the early 2000s, the racial gap in mortality rates stalled and then increased abruptly in 2020, coinciding with the onset of the COVID-19 pandemic, leaving the U.S. no better than it was in 1999, they said.
The study was published today in the Journal of the American Medical Association (JAMA).
To analyze trends in health disparities, the team examined U.S. death certificate data from the Centers for Disease Control and Prevention (CDC), comparing the age-adjusted mortality rates between the Black population and the white population. Separately, they estimated the excess years of potential life lost among the Black population—and the subsequent loss of human potential—by comparing the age of premature death against typical life expectancy.
“It is important to remember this is not an abstract concept. There is a real human toll to these entrenched inequities,” said Marcella Nunez-Smith, MD, MHS, associate dean for health equity research at Yale; C.N.H Long Professor of Internal Medicine, Public Health, and Management, and one of the authors. “The impact on families and communities should be unacceptable to all of us.”
“The results of the study are critically important,” said Harlan M. Krumholz, MD, Harold H. Hines, Jr. Professor of Medicine, professor of public health, director of the Yale-based Center for Outcomes Research and Evaluation (CORE), and senior author of the study.
“So far, our efforts to address health equity have failed to produce sustainable improvements in the lives and years lost by Black Americans because of disparities in death rates across the spectrum of age,” he said.
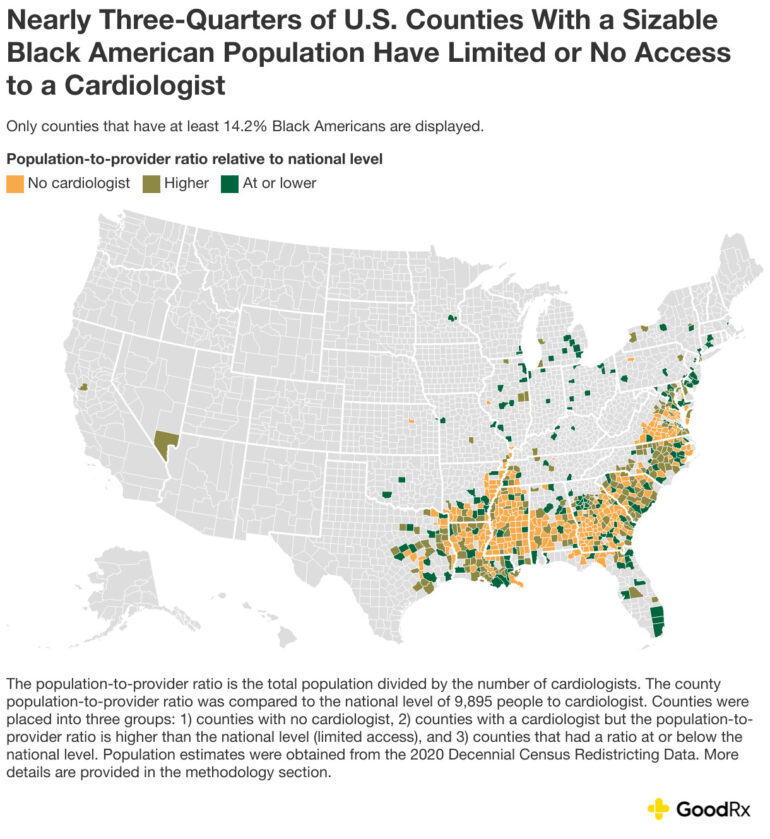
According to the analysis, heart disease was the number one contributor towards age-adjusted excess mortality for men and women, followed by cancer for men. The widest racial gap in years of potential life lost within the population occurs during the first year of life. Another finding was that after a brief period of progress, the COVID-19 pandemic had a disastrous impact.
“Despite initial progress during the early 2000s, we found persistent excess mortality rates among non-Hispanic Black adults,” said César Caraballo, MD, a postdoctoral associate at CORE and lead author of the study. “The abrupt worsening of these disparities in the first year of the pandemic indicates that current efforts to eliminate mortality disparities have been minimally effective and that progress has been fragile.
“We need targeted strategies aimed at early childhood health and preventing heart disease and cancer, some of the main drivers of these disparities, to build a more equitable future.”
More information:
César Caraballo et al, Excess Mortality and Years of Potential Life Lost Among the Black Population in the US, 1999-2020, JAMA (2023). DOI: 10.1001/jama.2023.7022
Citation:
Study documents staggering toll of health disparities for Black Americans (2023, May 17)