A One-Health review in East African countries shows that efforts to address antimicrobial resistance must go hand in hand with improved access to quality health care and antimicrobials.
Led by the Universities of Glasgow and Edinburgh, under a joint One Health Ph.D. studentship program, the review found that improving access to quality healthcare provision, of which antimicrobials are a major component, could help to address the risk of antimicrobial resistance in low- and middle-income countries.
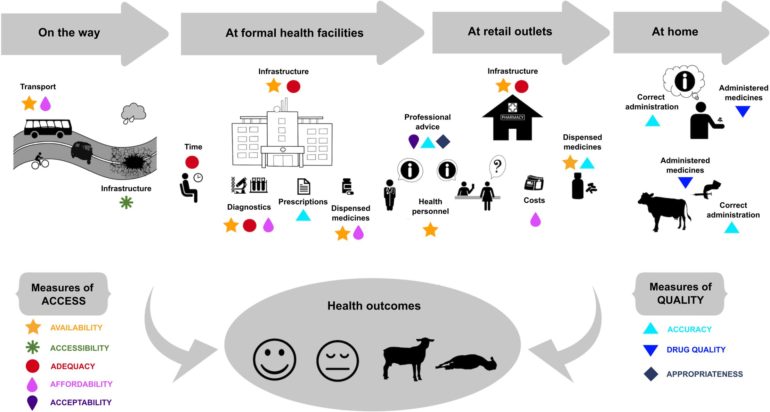
The review of research in East African countries, published in PLOS Neglected Tropical Diseases, found that a range of measures could help to balance the need for universal access to treatments with optimal use of medicines, in countries where limited access and uneven quality of care lead to potentially problematic practices around the use of antimicrobials in humans and livestock.
Their study of human and animal healthcare in Tanzania, Kenya and Uganda looked at previous research on the provision of widely used antimicrobial drugs, such as antibiotics and antimalarials.
The team, involving scientists from the University of Glasgow’s Institute of Biodiversity, Animal Health & Comparative Medicine and the School of Social & Political Sciences, and from the University of Edinburgh’s Roslin Institute, found infrastructural, economic, organizational and social barriers to human and animal healthcare at all levels of society.
The study found that human and animal healthcare coverage, including the availability of quality antimicrobials and counseling by trained professionals, is often inadequate, inaccessible and unaffordable. These issues are particularly acute in the most remote and disadvantaged communities where healthcare costs have a substantial impoverishing effect. Drug choice is often poorly informed, due to a ubiquitous lack of treatment and prescribing guidelines, training opportunities and diagnostic capacity to confirm the condition to treat.
Cost of treatment is also an important driver of treatment decisions. Underfunding and understaffing are widespread in public healthcare services, and supply issues lead to shortages of treatments, the review found. Combined, all of these factors can lead to antimicrobial overuse and over-prescription—a product of the major limitations of the healthcare system rather than inappropriate practices on the part of providers and users.
In a majorly constrained environment, informal care, comprising retail and community-based providers operating outside the formal system, critically compensates for these inadequacies and increases access to vital medicines. However, patients and farmers often do not have access to all necessary information on antimicrobial use, which can lead to suboptimal administration, dosing and course length.
To address the problem of antimicrobial resistance, the researchers suggest improvements to ensure that healthcare and medicines are good quality, affordable, available and accessible when necessary.
They also recommend the need to bring together all levels, from patients and farmers to healthcare providers and policy makers in order to understand the range of perspectives and constraints around health choices and practices key actors face, and how these could be addressed.
Future research should aim to better understand the link between human and veterinary use of antimicrobials to inform best practice for prescription, dispensing and use, and to examine antibiotic access for animal health. Such information can also facilitate the design and implementation of antimicrobial stewardship programs and resistance surveillance systems.
Overall, improvements to water and sanitation infrastructure as well as broader access to preventative interventions such as vaccination would reduce the high burden of infectious diseases, hence the need for antimicrobials in both humans and their livestock, the team concluded.
Dr. Tiziana Lembo, from the University of Glasgow’s Institute of Biodiversity, Animal Health & Comparative Medicine, said: “The antimicrobial resistance crisis exerts pressure on us to reduce the use of antimicrobials. Yet, in many African countries, the high burden of infectious diseases creates great dependence on these life-saving medicines. Problematic practices around antimicrobial use are largely the result of fundamental inadequacies of the health care system that limit the treatment choices people have. Enhancing access to high-quality health care would in the long run reduce risks of antimicrobial resistance, and improve people’s health and livelihoods.”
Dr. Adrian Muwonge, Roslin institute, said: “Antimicrobials are critical for health care delivery and have transformed how we produce proteins of animal origin globally. Therefore, we should do everything it takes to preserve their utility. We must invest in the infrastructure that delivers, preserves and protects the quality and accessibility of medicines, and promote appropriate dispensing, which is informed by diagnostics, as the foundation for good antimicrobial stewardship on the African continent.”
Reducing the use of critically important antimicrobials in pets
More information:
Kathrin Loosli et al, Addressing antimicrobial resistance by improving access and quality of care—A review of the literature from East Africa, PLOS Neglected Tropical Diseases (2021). DOI: 10.1371/journal.pntd.0009529
Provided by
University of Glasgow
Citation:
Better access to quality health care could curb antimicrobial resistance in East Africa (2021, July 23)
retrieved 25 July 2021
from https://medicalxpress.com/news/2021-07-access-quality-health-curb-antimicrobial.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.