Scientists from the International Livestock Research Institute (ILRI), the University of Liverpool, the University of Edinburgh and elsewhere have traced how livestock systems act as a reservoir for antimicrobial-resistant (AMR) bacteria and AMR genetic determinants that may infect or colonize people.
This sheds light on the factors influencing AMR at the intersection of multiple species and the One-Health sector. The study, undertaken in Nairobi, Kenya, appears in this week’s BMC Medicine, and helps detail how to avoid and manage the development of drug resistance in bacteria.
Alexander Fleming, who discovered the world’s first antibiotic, penicillin, warned that misusing antibiotics could lead to AMR. He showed that bacteria, viruses, fungi and parasites evolve when exposed to antibiotic drugs and eventually no longer respond to those medicines. As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become increasingly difficult or impossible to treat.
Today AMR can be found worldwide and is a serious problem. It has been estimated that unless the issue is tackled now, by 2050 one person will die every three seconds because of AMR.
“High-income countries can apply resources and large investments against AMR in ways which low-income countries can’t,” explained study lead scientist Dishon Muloi, a Research Fellow at the International Livestock Research Institute (ILRI) and former Ph.D. student at the University of Edinburgh.
“But AMR isn’t just a high-income problem or a low-income country problem. With the ease at which it can spread around the world, it’s everybody’s problem. So resistance in a community in Nairobi could actually mean clinical failures in a clinic in Hong Kong in two days or three days. We are not yet treating the problem with the urgency it needs, considering our connected world.”
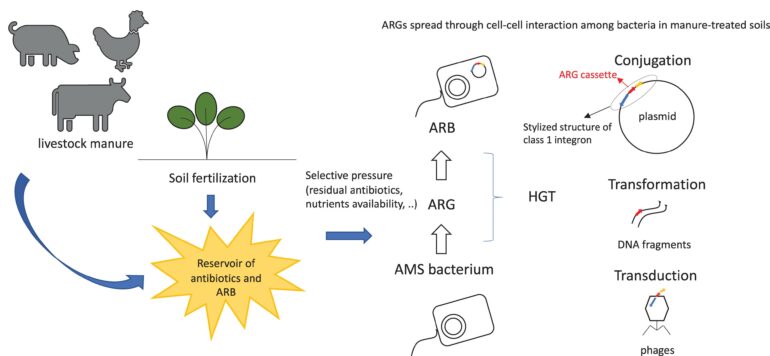
One path by which AMR is hypothesized to develop is through the large amount of antibiotics used in the livestock industry, where bacteria develop resistance and then spread to people. Quantifiable information addressing this has thus far been insufficient. Today’s study used genomics, epidemiology, and ecology to look into the patterns of AMR gene carriage in an exemplar organism, E. coli.
As part of a controlled epidemiological assessment of 99 households in Nairobi, Kenya, scientists sequenced the whole genomes of bacteria isolated from 311 human, 606 cattle, and 399 wildlife excrement samples. Using statistical models, they looked at the prevalence of AMR carriage and described the diversity and structure of the AMR genes in distinct host populations around the city. They also investigated conditions that could lead to the spread of AMR genes from humans to sympatric animals at the household level.
In animal and human isolates, the team found 13-point mutations and 56 acquired genes that are known to confer resistance to nine different antibiotic classes. They discovered that the makeup of the AMR gene community is not related to the host species, but that AMR genes were frequently co-located, possibly on plasmids, suggesting that multi-drug resistance could be acquired and spread in a single step. The risk for AMR transmission across human-livestock interfaces is greatest when manure is improperly disposed of, and in larger households.
Two policy implications flow from the study. The first is to highlight the importance of ecosystem-wide surveillance of AMR. “Doctors should not just be thinking about the rise of AMR in humans, but in livestock and the broader environment, because what we’re seeing is that wildlife collect and move around with what they acquire from the environment,” said Muloi.
The study’s findings of widespread carriage of clinically relevant AMR mechanisms in human and animal populations, especially in wildlife that move long-distances, underline the importance of evidence-based surveillance to combat antimicrobial resistance on a worldwide scale.
“This study shows how easily antimicrobial resistance genes move between humans and livestock in a crowded urban environment, underlining that if we are to beat the resistance problem we will need a coordinated response across the medical and veterinary sectors,” says Mark Woolhouse, professor and Chair of Infectious Disease Epidemiology, University of Edinburgh.
Second is the issue of manure disposal, which may seem mundane, but is essential. “If you drive around Nairobi, you see heaps of manure by the road,” said Muloi. “We haven’t traditionally thought of manure as a problem and even if we look at our policies, which are similar to those in many other countries, manure is not seen as a risk. But it’s clear we need to do a much better job of cleaning up the environment, for the sake of good public health.”
The study is part of an overall project called the Urban Zoo, or more formally known as the “Epidemiology, ecology and socio-economics of disease emergence in Nairobi.” The objective, says study lead Eric Fèvre, professor of veterinary infectious diseases, Institute of Infection, Veterinary and Ecological Sciences, University of Liverpool and jointly appointed principal scientist, ILRI, is to understand the mechanisms leading to the introduction and spread of pathogens into urban populations. “Here, we see that we need to take a holistic approach, which includes humans, animals, their waste and the shared environment,” says Fèvre.
More information:
Dishon M. Muloi et al, Genomic epidemiology of Escherichia coli: antimicrobial resistance through a One Health lens in sympatric humans, livestock and peri-domestic wildlife in Nairobi, Kenya, BMC Medicine (2022). DOI: 10.1186/s12916-022-02677-7
Provided by
International Livestock Research Institute
Citation:
How livestock systems act as a reservoir for antimicrobial-resistant bacteria (2022, December 9)