Monoclonal antibody drugs are among the few treatments available for COVID, providing a lifeline for those at high risk of severe illness and hospitalization. However, the usefulness of these drugs is limited because they are effective only when they can be administered early in the disease process.
In a new study, Rockefeller immunologist Jeffrey Ravetch and his colleagues altered currently available monoclonal antibodies for COVID using innovative approaches they have pioneered for the treatment of infectious and neoplastic diseases. In animal experiments, these altered antibodies proved more potent and protective against the virus compared to the ones being used today.
The findings, published in Nature, demonstrate how the treatment could be enhanced to make it suitable for treating more severe symptoms as well as effective at lower doses.
Optimizing monoclonal antibodies
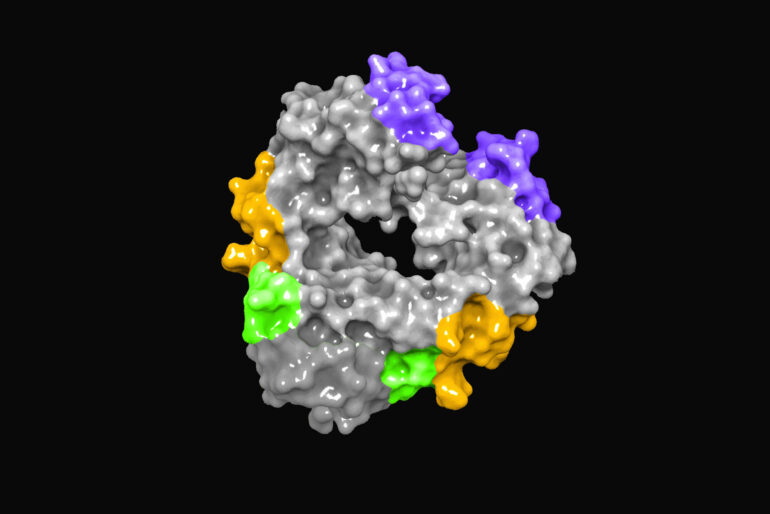
Antibodies are complex molecules consisting of multiple domains. The so-called Fab domain contains the antigen recognition site responsible for binding to targets such as a virus or an infected cell and can interfere with the ability of the virus to infect or be released from cells.
Antibodies also possess an Fc domain by which they alert the immune system to the presence of a threat. This portion of the molecule communicates with the rest of the immune system and affects the activities of nearly all immune cells by binding to a family of Fc receptors differentially expressed on the surface of these cells.
One set of Fc receptors, for example, can mediate the killing of infected cells and the clearing of virus particles, while another is responsible for activating T cells and triggering long-term immunologic memory. The Ravetch lab has previously shown that by understanding which Fc receptors are responsible for an antibody’s therapeutic activity, it is possible to re-engineer its Fc domain to optimize these activities and enhance the antibody’s potency and efficacy.
Recently, multiple groups have been investigating how monoclonal antibody treatments work to reduce disease severity in COVID with the goal of improving upon these treatments. Work on several other viruses has shown that the capacity to engage Fc receptors is an important factor in how protective such antibodies are.
“We have seen this before for Ebola, HIV, and influenza,” says Stylianos Bournazos, a research associate professor at Rockefeller. “Antibodies seem to lose their effectiveness in mice that lack Fc receptors or when modified to lose their ability to interact with these receptors.”
The antibodies currently in clinical use or in development for COVID treatment were selected primarily based on their ability to recognize the virus and limit its ability to infect cells. In the new study, Bournazos and his co-workers used a mouse model of SARS-CoV-2 infection to examine how these antibodies’ Fc domain contribute to their protective and therapeutic activity.
The Fc domain turned out to be essential, and when the antibodies were re-engineered to engage specific types of Fc receptors, they demonstrated increased protection in a mouse model of severe COVID.
The optimized anti-COVID antibodies are now being tested in clinical trials to determine if the findings from animal experiments might be applicable to the human disease.
“We hope that these enhanced molecules will provide better protection at lower doses than current antibody treatments and be effective at treating patients later in the disease course,” says Bournazos. “We expect that our Fc-optimized COVID antibodies will follow the rules established for other antibodies targeting tumors and other infectious diseases, where Fc enhancement generates superior clinical activity.”
More information:
Rachel Yamin et al, Fc-engineered antibody therapeutics with improved anti-SARS-CoV-2 efficacy, Nature (2021). DOI: 10.1038/s41586-021-04017-w
Provided by
Rockefeller University
Citation:
New design may boost potency of monoclonal antibodies against COVID (2021, November 19)