The p97 protein is one of your body’s best garbage disposers. It floats around in your cells looking for signals that a protein is past its shelf life and needs to be trashed. Mutations in this protein have been linked to neurodegenerative diseases, such as ALS and dementia, but p97’s relationship to these disorders is still being explored.
A study by researchers at Tufts University School of Medicine, published February 6 in Nature Communications, reveals some of the fundamental biology of p97, highlighting its role in ensuring our cellular organelles are in constant sync with one another.
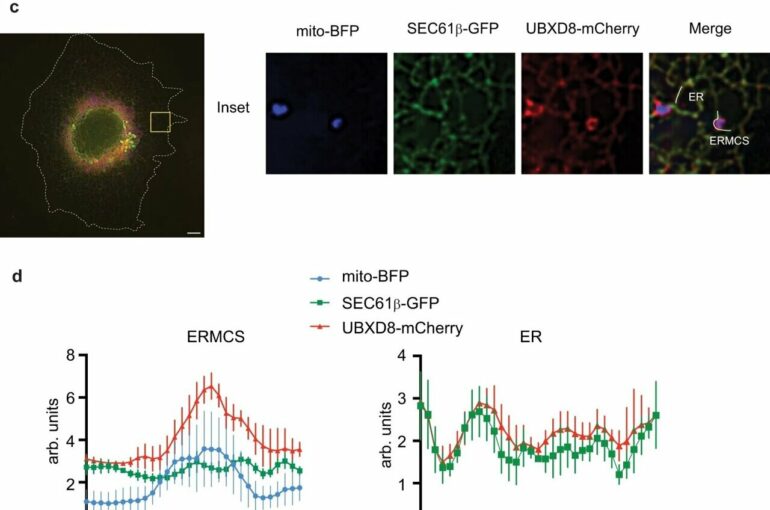
p97 works with numerous binding partners called co-factors, which help target p97 to proteins that need to be eliminated. The research team found that p97, in coordination with one of its co-factors UBXD8, help regulate the kinds of proteins present where a cell’s mitochondria (which produces energy for the cell) and endoplasmic reticulum (a network of membranes inside the cell that traffic proteins to different cellular destinations) connect.
These contacts, which allow the organelles to provide status updates or transfer cargo, are very sensitive to disturbances. When the p97-UBXD8 complex is absent, specific molecules accumulate on the endoplasmic reticulum membranes causing them to stick to the mitochondria.
However, what was surprising about their findings is that the molecules that collected at these contacts relayed information which caused the membranes to become more rigid. In fact, they found that if they could change the relative rigidity of the membranes at contacts, they could modulate how the contacts formed and dissipated.
“We’re always thinking about neurogenerative diseases caused by p97 mutation in terms of a protein not getting disposed and therefore accumulating and aggregating until it becomes a problem. But this study suggests that p97 mutation can also lead to miscommunication between organelles,” says senior author Malavika Raman, an assistant professor in the department of developmental, molecular and chemical biology at the School of Medicine.
“It’s important for organelles to make these minute-to-minute decisions, and so we’re really interested in trying to see how this communication goes awry in disease.”
To test whether what they were observing in lab dishes happens in animals, the research team used mouse models of p97 mutants that cause neurodegeneration. Their experiments confirmed that the proteins they found to be changing at organelle contacts were also altered in the brains of these mice, negatively impacting the interplay between the organelles.
“This is exciting because we have always thought about p97 mutations as a protein quality control defect, but now it appears that lipid metabolism may also be a significant contributor,” says first author Rakesh Ganji, a postdoctoral scholar in the Raman Lab. “Disruption of contacts and inherent lipid synthesis is emerging as a hallmark in a variety of human disorders such as neurodegeneration.”
The research team is next exploring what happens when human neurons have p97 mutations, and if there’s anything that can be done to help these neurons survive when organelle communication and protein disposal breaks down.
More information:
Rakesh Ganji et al, The p97-UBXD8 complex regulates ER-Mitochondria contact sites by altering membrane lipid saturation and composition, Nature Communications (2023). DOI: 10.1038/s41467-023-36298-2
Citation:
Study: Lipids can cause organelle miscommunication in neurodegenerative disease (2023, February 7)