The story of Candida auris starts in 2009, when a 70-year-old Japanese woman was admitted to the Tokyo Metropolitan Geriatric Hospital. Something discharges from one of her ears, and the doctors routinely take samples of it with a cotton swab. They analyze the sample to find out what is causing the infection.
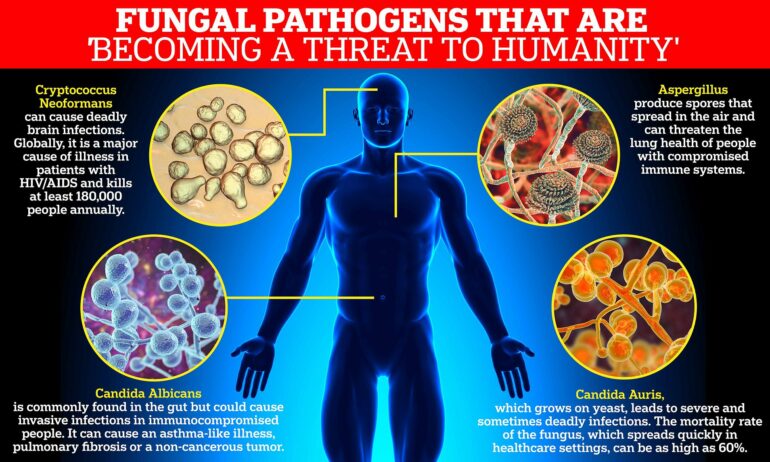
It turns out that a yeast is at play, and it’s different from other known yeasts. We are all familiar with baker’s yeast, a friendly microorganism, which is used to make beer and bred. Candida auris and other Candida yeast species are very different; they cause harmful and persistent infections, which are difficult to treat with known antibiotics.
Breakout in a London hospital
Against all expectations, Candida auris turns out to be unusually stress-resistant. The discovery is so unusual that the doctors decide to describe it in a scientific journal; they name it Candida auris after the place where it was found—auris means ear in Latin. Since then, the yeast has spread to all continents. Patients are almost always weakened people, and cases are almost always recorded in hospitals.
In 2015, for example, an acute infection with Candida auris ran out of control at the Royal Brompton Hospital in London. For three months, the staff tried everything to get rid of the infections, and finally they attempt a week-long spray attack. All surfaces in infected rooms were sprayed with hydrogen peroxide in the hope that the spray will reach all crevices and corners.
The spray device ran for a week, and to test if any microorganisms have survived, a gel-coated plate was then placed in the middle of the room. If any micro-organisms have survived the week-long spray attack, they would be attracted to the gel and thus reveal their existence. Only one organism appeared on the gel plate. Candida auris.
The first case in Denmark
In 2022, a Danish person returns home from South Africa to be admitted to a Danish hospital. The person has several wounds that need to be treated, and the South African doctors have discovered Candida auris on the patients’ skin.
The presence of a fungus on the skin is not in itself dangerous—it becomes so only when it enters the bloodstream—but the Danish hospital takes extra safety measures to ensure that Candida auris does not spread to other patients in the hospital: The patient is admitted to two rooms, so that there is also room for the equipment needed for examinations. This ensures that the patient does not have to be moved around to other departments.
To get to the two isolated rooms, staff has to go through two locks. The patient recovers and is discharged, and over a 24-hour period everything is disinfected in the rooms and in the locks.
Four cases in Denmark, so far
The next patient admitted to one of these two rooms stays there for only five hours—but that is enough for the patient to become infected with Candida auris in the bloodstream.
“It is difficult to understand how this could happen,” said Maiken Cavling Arendrup, professor and head of the Unit for Mycology, Statens Serum Institut in Denmark, who has followed the cases.
To date, four cases of Candida auris have been registered in Denmark, all from 2022. The three cases are on the skin of people who have returned home from abroad, while the fourth—the patient who was infected after five hours in the hospital room—was infected in the blood. Both the three carriers and the infected patient have recovered.
Need for better treatment
“The problem with this yeast is that it is very difficult to kill. It is multi-resistant, and thus you risk serious infections that cannot be treated,” said Maria Szomek from Daniel Wüstner’s research group, Department of Biochemistry and Molecular Biology.
“There are many types of medicine on the market that can fight fungal infections—including Candida auris. But they are becoming less and less effective, because Candida auris is extremely good at developing resistance, so the challenge now is to develop better medicines that work. This means medicine, which not only inhibits growth of yeast but actually kills any remaining yeast cells.”
Existing medicines against Candida auris and other yeasts with the potential to kill the cells are often based on so-called polyenes. Polyenes are a group of substances found naturally in certain bacteria as part of their inborn defense system. Polyenes can be extracted from the bacteria for medical use.
Can we improve nature’s own defense system?
But, as Maria Szomek points out; the mechanisms by which the polyenes kill yeast are not very well understood. This, however, is essential for developing new and improved polyene-based drugs.
“Therefore, we are working on understanding how nature’s own polyenes work,” Maria Szomek said.
This work takes place in Daniel Wüstner’s research group at the Department of Biochemistry and Molecular Biology. In their laboratory, the group uses advanced microscopy to study what happens to a yeast cell when attacked by polyenes. The group has teamed up with colleagues in theoretical and computational chemistry, Peter Reinholdt and Jacob Kongsted and is also working with two German research teams at Leipzig University and Humboldt University Berlin.
Precision attack in the cell
The researchers do not work with real Candida auris cells, but instead with harmless models, which they expose to polyenes from the fungicide Natamycin.
“We are interested in things like: how do the polyenes get through the cell membrane? How do they bind to and interact with ergosterol, which is a subgroup of steroids and the target of the polyenes’ attack,” Maria Szomek explained.
The group has described their latest study in Biochimica et Biophysica Acta (BBA)—Biomembranes.
More information:
Maria Szomek et al, Natamycin sequesters ergosterol and interferes with substrate transport by the lysine transporter Lyp1 from yeast, Biochimica et Biophysica Acta (BBA)—Biomembranes (2022). DOI: 10.1016/j.bbamem.2022.184012
Provided by
University of Southern Denmark
Citation:
Yeast fungus with the potential to become a global health problem (2022, November 3)