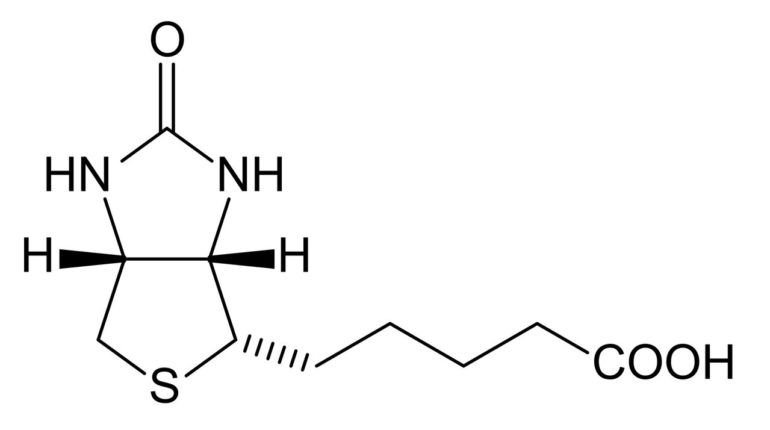
By any measure, carbon-based life originates from carboxylation. That is to say, the coupling of atmospheric carbon dioxide to sugar. Carboxylation is also critical for mitochondria to function. There are five carboxylation enzymes in mitochondria, and they share one thing in common—they are all operated by a covalently linked biotin cofactor.
Biotin is also known as vitamin H, named for the German words “Haar” and “Haut,” which mean hair and skin. This was due to the fact that even slight deficiencies cause hair thinning, skin rash or brittle fingernails. New research, just published in PNAS, now shows that some forms of severe neurodegeneration, like the frontotemporal dementia seen in Alzheimer’s and Parkinson’s, can directly result from lack of sufficient biotin.
The authors discovered this by looking at fruit flies with dementia. Now, before anyone chuckles, fruit flies actually make a nice model of Alzheimer’s or other diseases when they are given the right genes. Human versions of defective MAPT (tau) genes cause these flies to develop tauopathies that resemble those that occur in our own brains. To delve deeper into the neurotoxicity of tau, they looked at over 7,000 fly genes in a forward genetic screen before zeroing in on one significantly modified toxicity of the tauR406W mutant. This gene, Btnd, encodes the biotinidase enzyme that extracts biotin from food sources or recycles it from used enzymes.
Biotin comes to us in the form of biocytin, which is simply a biotin linked to a lysine. Btnd cleaves off the biotin from biocytin, or from its attachment to lysine in carboxylases. When Btnd was also crippled in the flies, their dementia got worse. Furthermore, their mitochondria also became deformed and elongated. The researchers were able to remedy all of these effects by simply giving supplementary biotin, suggesting that some humans with dementia could similarly benefit. They were also able to piece together a mechanism that functionally links tau and Btnd.
Although wayward variants of tau frequently wreak havoc in the cytoplasm of neurons by sticking together in hyperphosphorylated tangles, other tau isoforms are localized inside the nucleus where they can disrupt the organization of the heterochromatin. Heterochromatin consists mainly of tightly folded segments of chromosomes where idle genes are tightly stowed together. Disruption of these orderly structures will likely lead to aberrant expression of many genes. In the case at hand, the Brnd gene over in the p band in region 25 of chromosome 3 seems to have one particularly vulnerable locus.
Unfortunately, this is about as far as the authors could get in proving that this is exactly how everything goes down. However, as we reported yesterday, there are now potential ways to see firsthand whether the Brdn region has been molested by rogue tau. By targeting this locus with new, all-spatial in situ sequencing, the gene can not only be localized within the nucleus, but the folded state of the entire chromosome can be computationally reconstructed from the data. While such astounding capabilities would no doubt be handy, the bigger question for now is who, exactly, might benefit from biotin therapy?
On Tuesday we discussed mitochondrial misbehavior in the context of cancer, and noted that so-called rare variants are actually not very rare. It is only rare for people to know which variants they have when they are still asymptomatic and relatively healthy. The biotinidase Brnd is a great case in point. There are about 100 mutations already known to affect the function of the gene in one way or another. These are now continually tracked in a dedicated variant database chronicling Brnd insertions, duplications, deletions, splice anomalies, or sense, nonsense, and missense alterations.
Some of these mutations produce a nonfunction enzyme, or stop it from being made altogether, while others have seemingly little effect. Wikipedia tells us that “because the condition is inherited in an autosomal recessive pattern, two copies of the gene in each cell must be altered for a person to be affected by the disorder.” Wikipedia is lying to us. Any doctor who says something similar is lying to us. In fact, in spreading this myth of the unaffected carrier, science is lying to itself.
The truth is that if you have just one questionable variant, you are affected at some level whether you realize it yet or not. For example, if, at the age of 23, your Haar promptly thinned and your hairline receded by say, 50%, how would you be sure you were not affected? You might have your biotinidase enzyme activity measured in blood or skin cells and find it is better than 50%, but is that level really good enough for you? That strikeout in the bottom of the ninth back in 6th grade—might not a different fate have transpired but for a little biotin?
As mentioned above, there are five critical mitochondrial biotin-actuated carboxylases. It is worthwhile to list them:
AcetylCoA carboxylases 1 and 2 (or A and B), used in fatty acid synthesis and oxidation, respectivelyPyruvate carboxylase, used in gluconeogenesis PropionylCoA carboxylase, used in β-oxidation of fatty acidsMethylcrotonyl carboxylase, used in leucine catabolism
In order to know how much you are affected by variants in biotinidase, you also need to know about the activities of any variants you might have in any of these biotin-using enzymes. In principle, any further downstream variants within these pathways may also need to be figured into the rapidly diverging equation. The acetylCoA carboxylases have another dimension, which is interesting for us here. The mitochondrial isoform of ACC1 is required for the synthesis lipoic acid, which is another curious cofactor with many similarities to biotin.
For example, the structurally similar sulfur-containing biotin and lipoic acid are the only cofactors that are covalently bound to their parent enzyme—in both cases, at a lysine. Special arrangements for the synthesis of lipoic acid have been made in our cells. It was recently discovered that mitochondria maintain a bacterially derived fatty acid synthesis in order to generate the octanoic acid precusor to lipoic acid.
For now, who among us might benefit from taking biotin, and how much should be taken are still outstanding questions. We do know that if you have or suspect a deficiency, then raw egg whites, which contain high levels of unadulterated avidin, should be avoided, because they avidly bind to biotin.
FDA: biotin supplements could affect results of medical tests
More information:
Kelly M. Lohr et al. Biotin rescues mitochondrial dysfunction and neurotoxicity in a tauopathy model, Proceedings of the National Academy of Sciences (2020). DOI: 10.1073/pnas.1922392117
2021 Science X Network
Citation:
Biotin, mitochondria, and dementia: Research reveals a connection (2021, January 7)
retrieved 7 January 2021
from https://medicalxpress.com/news/2021-01-biotin-mitochondria-dementia-reveals.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.