Amidst a global pandemic, researchers are looking back in time at the only human disease we’ve ever successfully eradicated.
Even today, four decades after smallpox stopped circulating in the public, the disease is still regarded as one of history’s greatest killers, taking more lives for more centuries than any other single infectious disease, even plague and cholera.
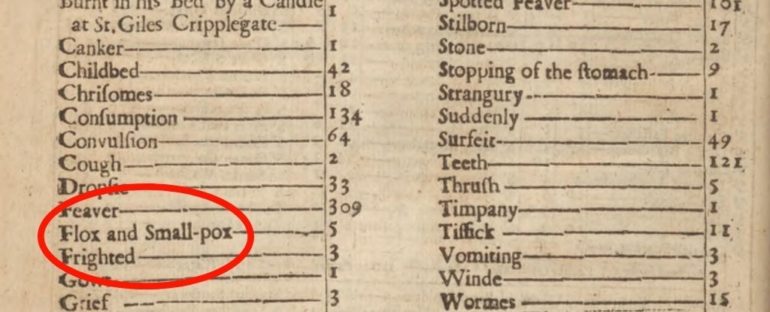
In the 18th century, 400,000 Europeans died each year from smallpox. In London alone, more than 321,000 people died from the disease post 1664.
A third of those who survived were left blind, and many more were disfigured by scars.
“The current COVID-19 pandemic has caused a surge of interest in the study of infectious disease transmission and how public health interventions could change the course of the pandemic,” says David Earn, who models infectious disease transmission at the McMaster University in Ontario.
“Our goal was to describe and make publicly available the weekly time series of smallpox mortality in London and to identify historical events that might have influenced smallpox dynamics over the centuries.”
For nearly 300 years, between 1664 and 1930, officials in London kept careful records of smallpox deaths. Digitising more than 13,000 of these weekly reports, researchers have created a major timeline of smallpox mortality and prevention, tracking the virus‘ movements in London and the ways in which it was influenced by seasons, public health policies and historical events.
Over time, the results clearly show that better control of the virus led to fewer smallpox deaths.
Outbreaks appeared sporadically in earlier records, settling into regular tides of infection by 1770 as a crude form of smallpox inoculation called variolation gained popularity.
Only in 1810, coinciding with the introduction of the far safer practice of vaccination, does the data show a dramatic reduction in the amplitude of epidemics, though outbreaks were more frequent and the data are noisier.”
A particularly large epidemic in 1830s London, which ultimately spread to Europe, was actually the impetus for England’s first Vaccination Act in 1840, giving free shots to anyone who wanted them and banning more dangerous practices like variolation. Only then did vaccination levels increase, with fatalities taking a downward plummet.
Other impacts like the seasonal structure of epidemics and the seasonal timing of outbreaks were more challenging to untangle, and the authors admit their data will need more investigation.
That said, the timeline is, to their knowledge, the longest weekly series of infectious disease mortality ever put together. As such, it helps illustrate how a virus can go from being “a terrifying and unavoidable danger” – killing roughly one out of every three people infected – to an extremely unusual cause of death.
From killer to rarity
In the years leading up to the last smallpox death in London, circa 1934, only a handful of deaths were reported from the virus.
“It is clear that the introduction of smallpox control measures – [inoculation] and later vaccination – made eradication possible,” says Olga Krylova, who worked on the project while studying mathematics and statistics at McMaster.
“Our analysis also suggests that greater use of control measures and changes in public health policies were correlated with changes in the frequency of the epidemics.”
Weekly smallpox mortality time series for London, England, 1664–1930. (Krylova and Earn, PLOS Biology, 2020)
Smallpox has a long and rich history, with current thinking associating it with a rodent disease that made the leap in Africa a few thousand years ago. Over millennia, as the world became more globalised, it appears this virus took off, spreading and growing alongside human civilisations and their trade routes.
In the Middle Ages of Europe, the virus frequently caused epidemics. Colonisation then spread it to Africa, Australia and North America.
Before the development of vaccines, people in Africa, India and China began relying on variolation to control the spread of smallpox. This entailed a small cut on the arm or leg, in which a tiny amount of the smallpox virus was introduced, taken from the pustules or scabs of those already infected.
The remarkable idea ultimately came to Europe in the 18th Century through trade with Turkey, and it was quickly taken up by physicians.
In 1796, a scientist by the name of Edward Jenner figured out that cowpox, which is born from a similar virus to smallpox, could protect humans against epidemics of this infectious disease. When he inoculated patients with this animal virus, it provided immunity in a safer, cheaper and more effective way than inoculation with the human virus.
By 1800, his work helped produce a smallpox vaccine in England. By 1840, inoculation was a thing of the past.
But that wasn’t the end of smallpox. It wasn’t until the late 19th century that scientists realised vaccine immunity was not lifelong and that people needed to be re-vaccinated.
After that, a global campaign from the World Health Organisation was able to successfully eradicate the virus in a decade. The last remaining samples are now stored in the US and Russia.
Throughout this long timeline, London was going through its own set of major cultural and historic changes. The Industrial Revolution, for instance, may have played a role in smallpox epidemics as urbanisation spread and social demographics changed. Wars were also another possible mechanism for spread.
“Further research using mathematical models is needed to quantify the impacts of interventions and historical events on the smallpox outbreaks,” says Krylova.
This extensive timeline can hopefully allow scientists to do just that. By honing in on specific events and their effects, we might come to better understand how contagious infections can fluctuate over time, and what we can do to beat them back in the end.
“The long history of documenting smallpox mortality in London provides an extraordinary opportunity to learn from the past about changing patterns in infectious disease transmission,” the authors conclude.
Now it’s time to dig into the data.
The study was published in PLOS Biology.