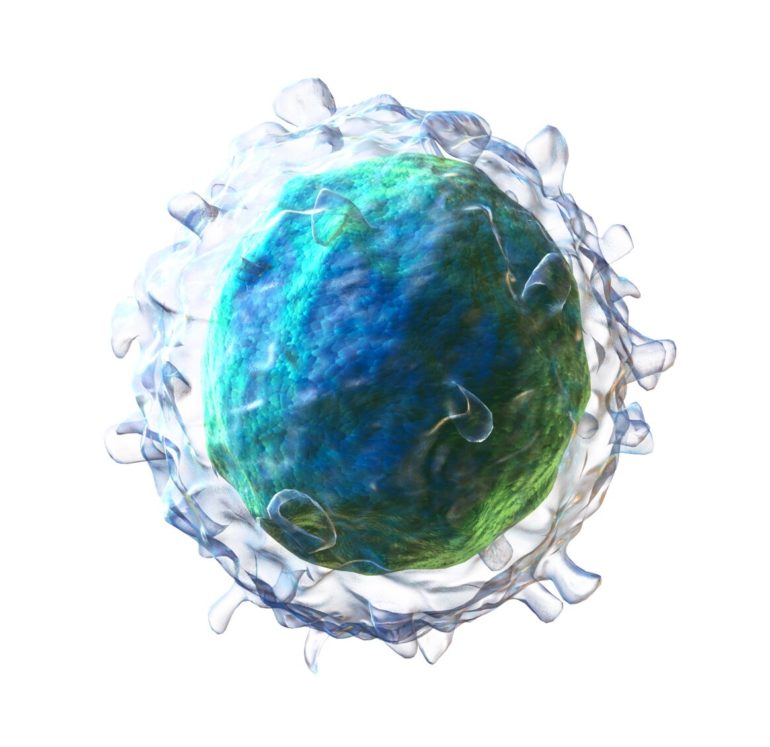
B cells are the immune cells responsible for creating antibodies, and most B cells, known as B2 cells, produce antibodies in response to a pathogen or a vaccine, providing defense and immunity against infections. But a small subset of long-lived B cells, known as B1 cells, are quite different from their short-lived cousins, the B2 cells. Instead of producing antibodies in response to invaders, they spontaneously make antibodies that perform vital housekeeping functions, such as removing waste like oxidized LDL cholesterol from the blood.
Like all the cells in the body, B1 and B2 cells have the same DNA, and therefore the same starting set of instructions. It is through epigenetic modifications, which open and close different areas of the genome to the machinery that reads the genetic instructions, that the same genome can be used to create unique instructions for each cell type. Understanding how the different epigenetic landscapes—the changes in instructions—allows for these differences in such similar cells is both an important fundamental question in immunology and can help scientists better understand diseases linked to B cells’ dysregulation.
Shiv Pillai, MD, Ph.D., a core member of the Ragon Institute of MGH, MIT and Harvard, studied the DNA modifications present in both cell types during different stages of development to identify an epigenetic signature that may determine whether a cell becomes a B1 or a B2 cell. This work was published recently in the journal Nature Communications.
“Through our analysis, we found the fate of a B cell is determined by epigenetic modifications driven by a protein called DNMT3A,” says Vinay Mahajan, MD, Ph.D., an instructor in Pathology at the Ragon Institute and the paper’s first author. “Genetic studies in humans link the genomic regions with these markers to a variety of immune-mediated disorders.”
The team studied CpG methylation, a type of epigenetic modification that opens up specific areas of DNA and marks regulatory elements that can turn genes on or off. They discovered a set of regulatory elements with unique features in these B1 and B2 cells. In most cases, CpG methylation is permanent and, once added, is even passed on when the cell replicates. But in B cells, the protein DNMT3A had to continually work to maintain these epigenetic modifications. If DNMT3A was removed from B1 cells, the epigenetic modifications were lost, and chronic lymphomic leukemia (CLL), a cancer caused by the uncontrolled replication of B1 cells, would arise.
“These unique B1 cells are vitally important to our ability to stay healthy,” says Pillai. “The antibodies they create help prevent clots and heart attacks. At the same time, understanding what genetic factors regulate them can help us better understand what happens when their regulation goes awry and leads to CLL and other diseases.”
A trait of the rare few whose bodies naturally control HIV: ‘Trained’ immune cells
More information:
Vinay S. Mahajan et al, B1a and B2 cells are characterized by distinct CpG modification states at DNMT3A-maintained enhancers, Nature Communications (2021). DOI: 10.1038/s41467-021-22458-9
Provided by
Massachusetts General Hospital
Citation:
Epigenetic changes drive the fate of a B cell (2021, May 13)
retrieved 13 May 2021
from https://medicalxpress.com/news/2021-05-epigenetic-fate-cell.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.