In the 20th century, when a routine infection was treated with a standard antibiotic, recovery was expected. But over time, the microbes responsible for these infections have evolved to evade the very drugs designed to eliminate them.
Each year, there are more than 2.8 million antibiotic-resistant infections in the United States, leading to over 35,000 deaths and US$4.6 billion in health care costs. As antibiotics become less effective, antimicrobial resistance poses an increasing threat to public health.
Antimicrobial resistance began to emerge as a serious threat in the 1940s with the rise of penicillin resistance. By the 1990s, it had escalated into a global concern. Decades later, critical questions still remain: How does antimicrobial resistance emerge, and how can scientists track the hidden changes leading to it? Why does resistance in some microbes remain undetected until an outbreak occurs? Filling these knowledge gaps is crucial to preventing future outbreaks, improving treatment outcomes and saving lives.
Antimicrobial resistance can be deadly.
Over the years, my work as a microbiologist and biomedical scientist has focused on investigating the genetics of infectious microbes. My colleagues and I identified a resistance gene previously undetected in the U.S. using genetic and computational methods that can help improve how scientists detect and track antimicrobial resistance.
Challenges of detecting resistance
Antimicrobial resistance is a natural process where microbes constantly evolve as a defense mechanism, acquiring genetic changes that enhance their survival.
Unfortunately, human activities can speed up this process. The overuse and misuse of antibiotics in health care, farming and the environment push bacteria to genetically change in ways that allow them to survive the drugs meant to kill them.
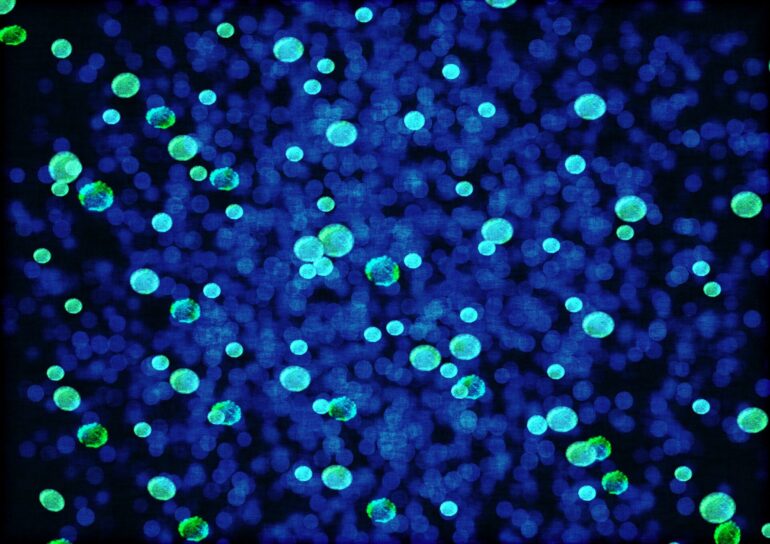
Early detection of antimicrobial resistance is crucial for effective treatment. Surveillance typically begins with a laboratory sample obtained from patients with suspected infections, which is then analyzed to identify potential antimicrobial resistance. Traditionally, this has been done using culture-based methods that involve exposing microbes to antibiotics in the lab and observing whether they survived to determine whether they were becoming resistant. Along with helping authorities and researchers monitor the spread of antimicrobial resistance, hospitals use this approach to decide on treatment plans.
However, culture-based approaches have some limitations. Resistant infections often go unnoticed until antibiotics fail, making both detection and intervention processes slow. Additionally, new resistance genes may escape detection altogether.
Genomics of antimicrobial resistance
To overcome these challenges, researchers have integrated genomic sequencing into antimicrobial resistance surveillance. Through whole-genome sequencing, we can…