Domestic violence, including intimate partner violence (IPV), before, during or after pregnancy is associated with many serious harms, including increased risk of maternal hemorrhage, higher rates of postpartum depression and increased risks of maternal and infant morbidity and mortality.
Universal screening for IPV during prenatal or postpartum health care visits is one of the most effective strategies for identifying and supporting people experiencing IPV, yet many IPV victims are not screened. Previous research has shown that IPV victims at the greatest risk for not being screened were Spanish-speaking Hispanic people, American Indian/Alaska Native people, people with Medicaid coverage and people with no health insurance.
A new study from the University of Minnesota School of Public Health (SPH) adds to this knowledge with an analysis of rural versus urban differences in rates of both IPV and IPV screening before, during and after pregnancy.
The study, which appears in Health Services Research, found:
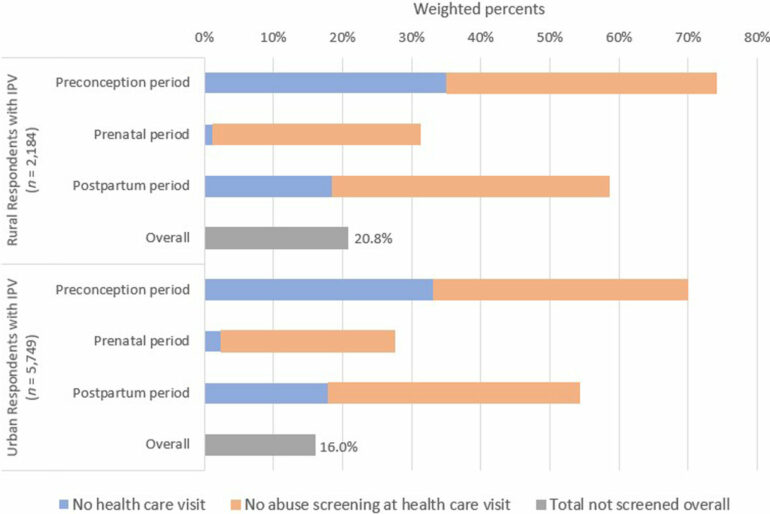
IPV is more common among rural birthing people than urban birthing people. Rural residents who were Medicaid beneficiaries, 18-35 years old, non-Hispanic white, Hispanic (English-speaking), or American Indian/Alaska Native had significantly higher predicted probabilities of experiencing perinatal IPV compared to their urban counterparts.Among respondents who experienced perinatal IPV, the predicted probability of not receiving abuse screening was 21.3% for rural and 16.5% for urban residents. Among rural IPV victims that were Medicaid beneficiaries, those who were 18-25 years old and those who were unmarried were at higher risk of not being screened for abuse compared to their urban counterparts.
“Intimate partner violence is a critical public health issue that affects thousands of birthing people across the country,” said Katy Backes Kozhimannil, lead author, professor at SPH, and director of Rural Health Programs at the Office of Academic Clinical Affairs.
“Screening by a health care professional is an effective strategy for identifying IPV around the time of pregnancy, and for getting victims the support and resources they need to be safe. Barriers to effective screening are exacerbated in rural areas where access to both health care and supportive services can be impeded by longer travel distances, workforce shortages and lack of local IPV resources.”
“In order to adequately address this health problem, policymakers, health care clinicians, social services providers and other stakeholders should invest in rural communities to ensure the safety of rural families.”
The researchers recommend that efforts to address IPV among rural residents should focus on universal abuse screening during health care visits, continuous health insurance coverage and targeted support for at-risk people in rural communities—before, during and after pregnancy.
Future research on identifying IPV-related consequences—including cases at particularly high risk for maternal and infant mortality—as well as efforts to improve IPV prevention, detection, support services and harm reduction, should also assess and address differences for rural and urban residents.
More information:
Katy Backes Kozhimannil et al, Rural/urban differences in rates and predictors of intimate partner violence and abuse screening among pregnant and postpartum United States residents, Health Services Research (2023). DOI: 10.1111/1475-6773.14212
Provided by
University of Minnesota
Citation:
Intimate partner violence before or during pregnancy more common among rural residents, finds study (2023, August 23)