A strain of the bacterium Klebsiella pneumoniae isolated from an 86-year-old woman with a urinary infection admitted to hospital in Brazil’s Northeast region in 2022 proved resistant to all available antibiotics. The patient died 24 hours after being hospitalized.
A group of researchers sequenced the bacterium’s genome and compared it with a database of 48 similar sequences. Alarmingly, the results showed that the strain in question had previously been detected in the United States, was already circulating in Brazil, and could potentially spread around the world.
The study is published in The Lancet Microbe.
“The bacterium is so versatile that it adapts to changes in treatment, easily acquiring resistance mechanisms not targeted by existing drugs either singly or in combination. It could become endemic to health care facilities worldwide,” said Nilton Lincopan, last author of the article and a professor at the University of São Paulo’s Biomedical Sciences Institute (ICB-USP) in Brazil.
Lincopan runs One Health Brazilian Resistance (OneBR), a database with epidemiological, phenotypical and genomic data on bacteria classified as “critical priority pathogens” by the World Health Organization (WHO).
This classification encompasses bacteria for which few therapeutic options are available, that merit containment measures to prevent dissemination, and that should be prioritized for the purposes of research and development of novel antimicrobials.
OneBR’s database currently holds 700 genomes of human and animal pathogens.
Health services are required to notify the local epidemiological surveillance authority when multidrug-resistant strains like this are detected. The patient must be isolated, and all health workers involved must take extra precautions to prevent transmission of the pathogen to other patients.
“As an opportunistic pathogen, the bacterium may not cause disease in patients with normal immunity, but in people with low immunity, it can cause severe infections. In the hospital environment, patients in intensive care units [ICUs] or being treated for other diseases can acquire a secondary infection such as pneumonia. With no treatment available and with a depressed immune system, they often die,” Lincopan said.
Favored by the pandemic
The authors note that a rapid increase in pan-beta-lactam-resistant K. pneumoniae co-producing carbapenemases was observed across Latin America and the Caribbean during the COVID-19 pandemic. Carbapenemases are enzymes that hydrolyze most antimicrobial compounds, making them ineffective. Beta-lactams are the most widely used class of antibiotics.
The spread of these bacteria was reported to the Pan American Health Organization (PAHO) and WHO, which issued an epidemiological alert.
A global genomic analysis published recently by a group led by Fábio Sellera, a professor at the Metropolitan University of Santos (UNIMES) in Brazil, also reported rapid growth in multidrug-resistant bacteria, stressing that the high prevalence of K. pneumoniae strains indicates a novel resistance trend and a serious public health threat.
An antibiotic combining a third-generation cephalosporin, ceftazidime, with a new beta-lactamase inhibitor, avibactam, was approved by the United States Food and Drug Administration (FDA) in 2015 and is indicated for treatment of K. pneumoniae carbapenemase (KPC)-producing bacteria.
Ceftazidime/avibactam was approved by ANVISA, the Brazilian equivalent of the FDA, in 2018 in view of the large number of reported KPC infections.
“Hospitalization of people with COVID-19 associated with secondary infections by this type of bacterium probably led to a global increase in the use of ceftazidime/avibactam, favoring the emergence of strains resistant to this new antibiotic,” Lincopan said.
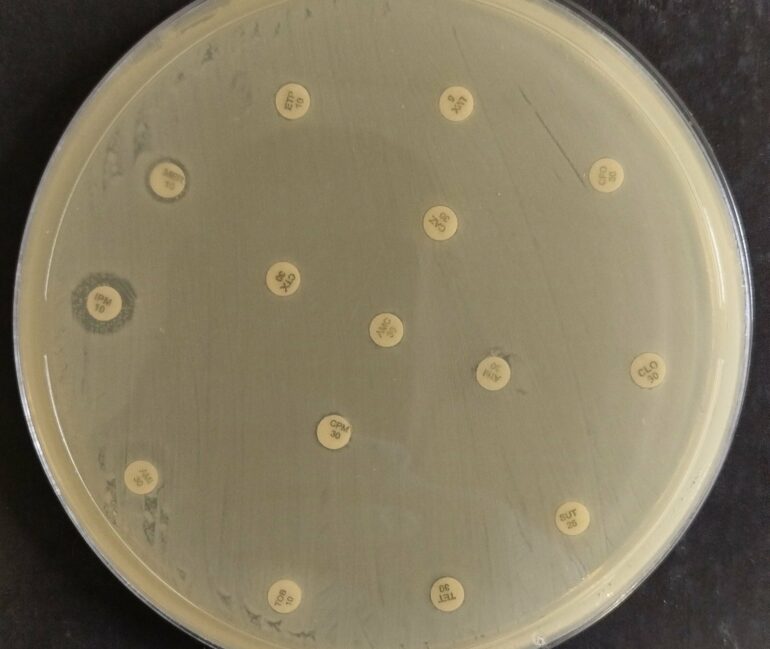
The standard procedure for patients hospitalized with suspected bacterial infections would be to collect clinical material for confirmation of the diagnosis and testing of susceptibility to the different antimicrobials available.
“KPC-producing strains treated with ceftazidime/avibactam probably evolved rapidly, acquiring resistance to this latest therapeutic option. We now have carbapenemase co-producing strains that don’t respond to treatment with beta-lactams,” he said.
Besides the need for permanent monitoring of the pathogenic bacteria found in hospitals, the researchers also stress the importance of rational prescribing of antibiotics. The message for patients is that when antibiotics are prescribed they must adhere to the full course of treatment even if they feel well after two or three days. This will also avoid the emergence of more drug-resistant strains.
The first author of the article was Felipe Vásquez Ponce, a Ph.D. candidate at ICB-USP. The study was also supported by Johana Becerra, a researcher at ICB-USP and a member of the OneBR team.
More information:
Felipe Vásquez-Ponce et al, Global epidemiological trend of Klebsiella pneumoniae ST340: emergence of subclade KL15 co-producing K pneumoniae carbapenemase-2 and New Delhi metallo-β-lactamase-7 in the Americas, The Lancet Microbe (2024). DOI: 10.1016/j.lanmic.2024.100990
Citation:
Multidrug-resistant strain of K. pneumoniae detected in Northeast Brazil (2024, November 12)