A new study urges that state and federal regulators need to take a closer look at health and safety risks of the growing medicinal and recreational cannabis market.
“Cannabis regulation is unlike any agricultural commodities, food, or drugs in the U.S. Currently, there are no national-level guidelines based on conventional risk assessment methodologies or knowledge of patients’ susceptibility in medical use of cannabis,” said lead author Max Leung, an Arizona State University assistant professor in the School of Mathematical and Natural Sciences.
“Therefore, our research team conducted the first comprehensive study to examine 3 main concerns: 1) the current landscape of state-level contaminant regulations, 2) identifying cannabis contaminants of concern in samples, and 3) explore any patient populations who may be susceptible to contaminants.”
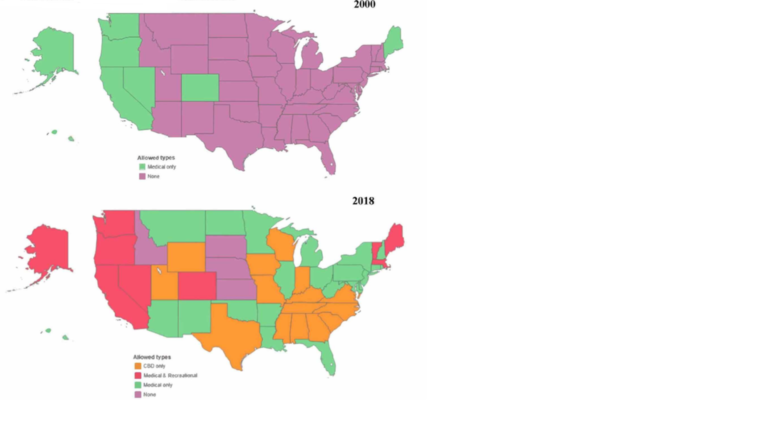
The cannabis market has grown significantly in the past decade to become a $10 billion industry by 2017, $50 billion in 2026, and, within the past year, an estimated 55 million users. Currently, 15 states have made medicinal cannabis legal, but little attention has been paid to its implications in chemical exposure and consumer safety.
At the federal level, cannabis is still listed as an illegal substance. This limits the efforts of several federal agencies in assessing and mitigating the public health risk of cannabis contamination. Currently, cannabis is neither federally regulated as an agricultural, food, nor pharmaceutical commodity, so the USDA does not monitor its growth and FDA does not consider it a drug.
So, how is a cannabis user to know what they are putting into their bodies is safe? “There is surprisingly limited information on the contaminant level of cannabis products sold in this country,” said Leung.
Without any federal guidelines, it’s been left entirely up to the states to craft a patchwork of cannabis regulations and policy. “Individual legalized states and D.C. set their own rules with huge discrepancies,” said Leung.
From their study, Leung and colleagues found that as of May 2022, 36 states and the District of Columbia have listed a total of 679 cannabis contaminants listed as regulated in medical or recreational cannabis. Most of these contaminants were pesticides (551, which included 174 insecticide, 160 herbicide and 123 fungicides subcategories), followed by solvents (74), microbes (21), inorganic compounds (12), mycotoxins (5) and 16 classified as “other.”
“What was interesting is that many pesticides in this document were highly unlikely to be utilized in cannabis cultivation and processing,” said Leung. These pesticides included chlorpropham (a plant hormone that prevents potatoes from sprouting), oxytetracycline (an antibiotic), and norflurazon (an aquatic herbicide for Hydrilla control).
“What was also alarming to us is that the U.S. EPA tolerance document and individual jurisdictions also listed a total of 42 legacy pesticides that were no longer registered for any agricultural use in the U.S., such as dichlorodiphenyltrichloroethane (DDT), chlordane, lindane and parathion.”
As to the amount of contaminants levels, there were large inconsistencies from state to state. different state jurisdictions showed significant variations in regulated contaminants and action levels ranging up to four orders of magnitude.
How often was this a problem? The research team also mined data testing records of cannabis flower and extract samples produced in California, the largest state cannabis market in the U.S. Their sample data represented about 6% of California’s legal production in 2020-2021.
“As mandated by California’s Medicinal and Adult-Use Cannabis Regulation and Safety Act, all cannabis and cannabis products in the legal market of California are required to be tested for 68 pesticides, four inorganics, 20 solvents, six microbes, and five mycotoxins,” said Leung.
“The cannabis manufacturers must submit their products—including cannabis flowers and cannabis products such as edibles, concentrates, and other consumables—to a state-licensed cannabis testing laboratory. All products must be certified for compliance testing before they can be sold legally. The products that failed the state’s regulatory levels in the compliance testing are subject to recalls.”
The tallied an overall failure rate of 5.1% for the California cannabis samples, which included an average of the failure rate of 2.3% identified for flowers and 9.2% for extracts in California samples. Insecticides and fungicides were the most prevalent categories of detected contaminants, with boscalid and chlorpyrifos being the most common. The contaminant concentrations fell below the regulatory action levels in many legalized jurisdictions, indicating a higher risk of contaminant exposure.
Lastly, Leung’s team reviewed the medical cannabis use reports released by state-level public health agencies from 2016 to 2021. Currently, there are 37 U.S. medical cannabis programs in and close to a hundred qualifying medical conditions listed by these programs.
“Cannabis and cannabis products are often marketed as alternative options to standard medical treatments,” said Leung. “As such, medical cannabis can potentially expose susceptible patients to harmful contaminants.”
“Immunocompromised patients with cancer and HIV, women of reproductive age, and patients with seizures and epilepsy are among those who are more susceptible to the health hazards of pesticide and microbial contaminants that may be found in cannabis,” added Leung.
The majority of patients were prescribed medical cannabis for use in alleviating pain (799,808 patients), followed by post-traumatic stress disorder (164,383 patients), spasticity associated with multiple sclerosis or spinal cord injury (78,145 patients), cancer (44,318 patients), and epilepsy (21,195 patients).
“Our findings have two important public health implications,” said Leung. “First, the scattershot approach of regulations at the state level can confuse cannabis manufacturers and discourage compliance while subjecting cannabis users to a higher level of contaminant exposure in some jurisdictions. Second, given the current status of cannabis contaminant regulation in the U.S., it is unclear whether the health benefit of cannabis usage outweighs the health risk of exposure to cannabis-borne contaminants.”
To help better inform the public and policy makers, Leung recommends further investigations to examine the safety considerations in susceptible patient populations across all medical conditions.
“The progression and prognosis of many qualifying conditions may be worsened by exposure to detected contaminants in cannabis,” said Leung. “This study demonstrates an urgent need for a unified regulatory approach to mitigate the public health risk of cannabis contamination at a national level.”
The study, “Comparison of State-Level Regulations for Cannabis Contaminants and Implications for Public Health”, was published online September 14 in the peer-reviewed journal Environmental Health Perspectives.
More information:
Comparison of State-Level Regulations for Cannabis Contaminants and Implications for Public Health, Environmental Health Perspectives (2022). DOI: 10.1289/EHP11206
Provided by
Arizona State University
Citation:
Study examines current state regulations, public health risks of growing medicinal and recreational marijuana market (2022, September 14)