People who smoke cigarettes and automatically receive help to quit are more likely to succeed, even if they aren’t fully motivated at first. A new study led by researchers at The University of Kansas Cancer Center found that an opt-out approach, where people who smoke are provided with tobacco cessation medications and counseling unless they decline, significantly increases quit rates. One month after starting, 22% of people in the opt-out group had quit smoking, while only 16% in the opt-in group had quit. Their findings were recently published in JAMA Network Open.
The study was conducted with people who smoked and were patients at The University of Kansas Health System. Participants were randomly placed into one of two groups: opt-out or opt-in treatment. In the opt-out group, unless they declined, patients automatically received all components of evidence-based tobacco treatment including a starter kit of nicotine patches and gum, a prescription for quit smoking medication, a treatment plan, and follow-up calls.
Opt-out patients were free to decline (“opt-out” from) any component of care. In the opt-in group, patients were asked if they would like each treatment component and only got the components they agreed to receive.
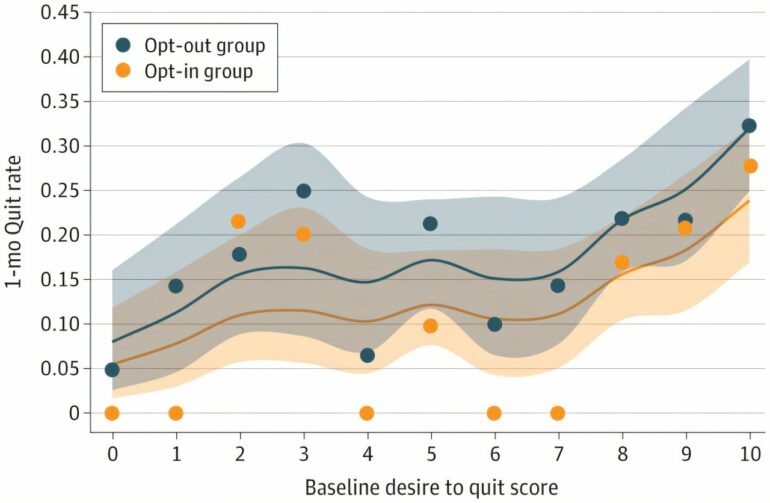
Patients were asked to choose a number between 0 and 10 to measure their desire to quit. Zero meant they were not thinking about quitting, and 10 meant they were taking action to quit. The researchers then used Bayesian statistical methods to see how the desire to quit affected the chances of quitting, comparing opt-out to opt-in treatments.
Byron Gajewski, Ph.D., professor of Biostatistics and Data Science and co-director of KU Cancer Center’s Biostatistics and Informatics Shared Resource, co-authored the paper with Babalola Faseru, MD, and Kimber Richter, Ph.D., both professors of Population Health. All three are members of KU Cancer Center’s Cancer Prevention and Control research program.
The team leveraged The University of Kansas Health System’s UKanQuit program, which is a bedside tobacco treatment service, to conduct the study. UKanQuit has served as a foundation for several major clinical trials aimed at finding the most effective methods to engage smokers in cessation programs before they are discharged from the hospital.
“Health care providers don’t ask patients if they would like to get evidence-based care for other conditions like asthma, high blood pressure or diabetes,” said Dr. Richter. “They just identify a health condition and provide the best care possible. For no reason, we’ve always treated tobacco dependence differently—we wanted to see what would happen if we proactively treated tobacco dependence.”
Out of 739 participants, the study showed that in both groups, smokers who were ready to quit were more likely to quit. However, at every level of motivation, smokers were more likely to quit if they received opt-out care than if they received opt-in care. Overall, the benefit of opt-out treatment stayed the same, no matter how much the person wanted to quit when they started.
“This study is significant because it shows that proactively providing help without requiring a strong initial desire to quit can still make a big difference,” said Dr. Gajewski. “It suggests that opt-out treatment could be an effective strategy to help more people quit smoking.”
More information:
Byron Gajewski et al, Desire to Quit Smoking, Opt-Out Tobacco Treatment, and Cessation, JAMA Network Open (2024). DOI: 10.1001/jamanetworkopen.2024.33802
Provided by
University of Kansas Cancer Center
Citation:
Study finds opt-out treatment helps smokers quit, even those with low motivation (2024, October 21)