New work has disclosed significant findings on the survival of the Legionella pneumophila bacterium in hospital water systems. Recently published in the journal Science of The Total Environment, the study suggests adjustments to control policies to effectively combat legionellosis.
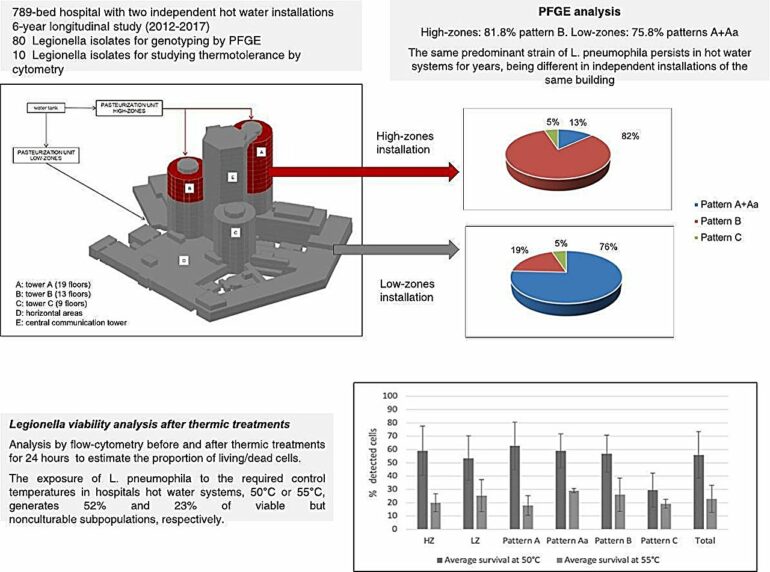
The study examined 80 isolates of Legionella pneumophila serogroup 6 from two independent hot water systems in a hospital, highlighting the genotypic variability and thermotolerance of the strains. By using flow cytometry to assess membrane integrity after exposing the bacteria to temperatures of 50°C, 55°C, and 60°C for 24 hours, the team found that a significant percentage of bacteria showed no growth on plate cultures, but remained in a viable but non-culturable (VBNC) state.
Specifically, 52% of the bacteria at 50°C and 23% at 55°C retained their membrane integrity, while less than 5% did so at 60°C. These findings underscore the limitation of the plate culture method for detecting Legionella under thermal stress conditions.
The research team includes the Clinical and Environmental Infectious Diseases Study Group (CEID) at Germans Trias i Pujol Research Institute (IGTP), led by Dr. Laura Gavaldà from the Bellvitge University Hospital, in collaboration with Institut Català d’Oncologia and Barcelona Public Health Agency.
Noemí Párraga, the first author of the study, emphasizes, “The plate culture technique for Legionella control, required by Spanish legislation, underestimates the presence of this bacteria under stress factors, as it may remain in a viable but non-culturable state. This state can be reversed, recovering the microorganism’s infective capability.”
This study suggests the possibility of improving detection methods to ensure safe hospital environments, acknowledging that Legionella can withstand regulatory temperatures and remain in a viable but non-culturable state. It is advisable to consider this subpopulation in assessments, as it has the potential to become infectious.
“Increasing the temperature by 5˚C at the endpoints of hot water circuits could significantly reduce cases of legionellosis, especially in centers with a high presence of at-risk individuals,” points out Dr. Gavaldà.
In 2022, the new Royal Decree 487/2022 was published in Spain, establishing the sanitary requirements for the prevention and control of legionellosis. This document sets out a series of measures for the prevention and control of Legionella in water installations. One of the defined measures is the temperature in hot and cold water circuits. A minimum temperature of 60°C is established in accumulators and 50°C at the endpoints (taps and showers) and on the return. The minimum required by the current royal decree are the microbiological controls through plate culture.
Dr. Laura Gavaldà was a specialist in the Preventive Medicine and Hospital Hygiene Service at Bellvitge Hospital at the time of the study. She is currently the head of the Tuberculosis Prevention and Control Service and Specific Programs at the Public Health Agency of Catalonia.
More information:
Noemí Párraga-Niño et al, Persistence of viable but nonculturable Legionella pneumophila state in hospital water systems: A hidden enemy?, Science of The Total Environment (2024). DOI: 10.1016/j.scitotenv.2024.172410
Provided by
Germans Trias i Pujol Research Institute
Citation:
Study reveals need to review temperature control measures in hospitals to manage Legionella (2024, May 10)