When seemingly healthy people receive an alert from a wearable sensor telling them they might have a respiratory virus—based on small changes in their unique heart rate, sleep and activity patterns—what do they do? According to a new study by Scripps Research scientists carried out at the height of the COVID-19 pandemic, only a quarter of people follow up such an alert with an at-home viral test.
That is just one conclusion of the new study, published in The Lancet Digital Health on July 24, 2024, which tested the feasibility of using wearable sensors and associated alerts to guide people’s behavior. The paper is titled “Wearable sensor signals and self-reported symptoms to prompt at-home testing for acute respiratory viruses: a digitally-enabled pilot randomized clinical trial.”
The findings also underscore the importance of timing alerts correctly and communicating them in a personalized manner, which has broad implications for designing and clinically implementing new wearable sensors that track everything from infections and blood sugar levels to women’s menstrual cycles or pregnancies.
“What was exciting about this study is that we showed we can provide an individualized infection alert based on data passively monitored by sensors,” says first author Giorgio Quer, Ph.D., director of artificial intelligence at Scripps Research Translational Institute and assistant professor of Digital Medicine at Scripps Research, “and we understood the main limitations in providing this alert to participants. We need to keep in mind how to communicate these changes to people so that they lead to actionable behavior changes.”
In a previous study, Quer and his colleagues discovered that data from wearable fitness and health monitors could be used to identify—with roughly 80% accuracy—whether a person was likely to have COVID-19. More sleep, less activity, and a higher resting heart rate than usual was associated with having a respiratory infection.
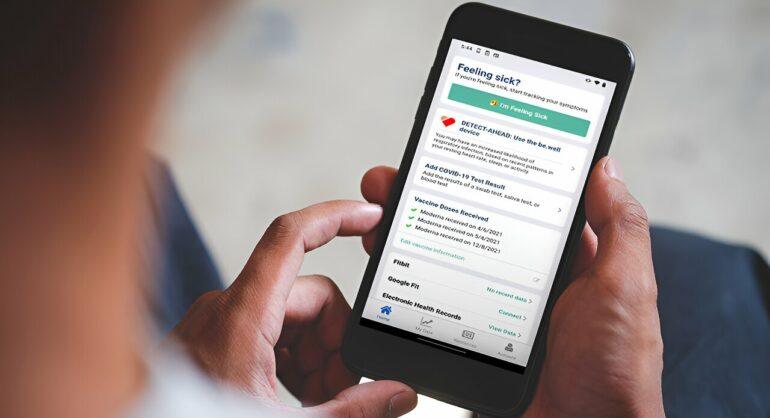
In the new study, Quer’s team tested whether alerting people to these changes could prompt them to take at-home self-tests for COVID-19 and respiratory syncytial virus (RSV), even if they did not have symptoms yet.
Between September and December of 2021, the researchers enrolled 450 adults living in the U.S. Participants were divided into three groups: those who received alerts prompting them to test based on changes detected by a wearable sensor or symptoms (both the sensor and viral tests were provided), those who received alerts based only on reported symptoms, and those who did not receive alerts or tests.
“There are both individual and public health benefits to alerting people of early physiological changes that might signal a viral infection,” says Steven Steinhubl, MD, senior author, adjunct at Scripps Research and professor of Biomedical Engineering at Purdue University. “It can give people extra time to isolate, change their plans and prevent spreading the virus.”
Over the course of the study, 118 participants (39%) were prompted to self-test at least once, with 62 of those people (52%) successfully carrying out the self-test and recording the results.
People were more often prompted to self-test because of symptoms and were more likely to self-test if they had symptoms; 23% of those prompted to test due to changes in sensor data actually tested, while 56% tested when prompted due to their symptoms.
One reason the researchers suspect this trend: Alerts based only on sensor data were delivered at a fixed time of the morning, when people may not have been readily available to test. Alerts based on symptoms, however, were delivered at the same time symptoms were reported, when people were likely thinking about the possibility of a virus and had a few minutes free.
“This is something that we think is really important to keep in mind for future studies on wearable health monitoring,” says Quer. “The timing with which you alert people to changes in their health is really critical if you want to ultimately impact behavior.”
Among the other takeaways from the digital health feasibility trial: It was possible for the researchers to recruit a very diverse population since they did not require any in-person visits to medical centers or clinicians. But finding infection information in the provided electronic medical records turned out to be more difficult than expected.
Quer says these kinds of lessons are key to developing future studies using wearable health monitors. His team is studying, for instance, whether sensors can help alert pregnant women to any increased risk of health complications like gestational diabetes, pre-eclampsia or preterm deliveries.
“We need to study not only how to make these kinds of predictions, but how to return information to patients in a way that is useful,” he says.
More information:
Giorgio Quer et al, Feasibility of wearable sensor signals and self-reported symptoms to prompt at-home testing for acute respiratory viruses in the USA (DETECT-AHEAD): a decentralised, randomised controlled trial, The Lancet Digital Health (2024). DOI: 10.1016/S2589-7500(24)00096-7. www.thelancet.com/journals/lan … (24)00096-7/fulltext
Provided by
The Scripps Research Institute
Citation:
Timing matters: Study suggests ways to improve wearable sensor health alerts (2024, July 25)