Scientists working on a lab-grown mini-lung are now using their living model to better understand the current pandemic and potential new treatments.
The most recent version of this unique organoid is based entirely on human stem cells, known to repair the deepest parts of our lungs. When the researchers exposed it to SARS-CoV-2, the results were illuminating.
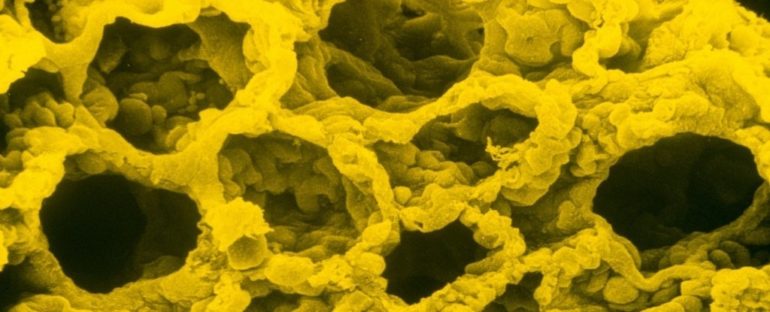
Dropping just one of these self-renewing units into a dish containing a tailored growth solution can produce millions of cells in a clump that resembles the tiny air sacs in human lungs.
Known as alveoli, these balloon-like sacs have shown diffuse damage in fatal cases of COVID-19, and while this havoc is often attributed to a storm of immune cells called cytokines, we’re still figuring out how lung injury actually comes about.
The new mini-model gives us a glimpse of the battle on a molecular scale, and while it’s nowhere near as complex as a real human lung, that’s also what makes it easier to control and observe.
The unique organoid includes just one type of lung stem cell, known as an alveolar type 2 epithelial cell (AT2), which has the ability to self-renew, differentiate into other lung cells, keep the sac open with surfactants, and directly bind to viruses.
When the SARS-CoV-2 virus was introduced into this organoid’s dish, researchers say the virus quickly infected the AT2 cells and spread throughout the alveoli-like structure.
The infection also triggered an inflammatory response in the organoid, reducing the production and proliferation of surfactant and inducing cell death, sometimes in surrounding areas that hadn’t even yet been touched by the virus.
“This is a major breakthrough for the field because we were using cells that didn’t have purified cultures,” explains Ralph Baric, an epidemiologist, microbiologist, and immunologist at the University of North Carolina.
“This is incredibly elegant work to figure out how to purify and grow AT2 cells in culture.”
Analysing the gene expression of these mini-organs, researchers found the inflammatory state triggered by the SARS-CoV-2 infection led to the production of interferons, cytokines, chemokines, and activation of genes related to cell death.
What’s more, these signatures showed “striking similarity” to what’s seen in severe COVID-19 patients. The results also match recent growing evidence that suggests severe cases of COVID-19 trigger a cytokine storm that may leave the lungs susceptible to damage.
Most of these observations, however, come from autopsies and have not been observed in living tissue.
This newly-developed model is a unique and versatile new way to study respiratory viruses in action, and it shows how a cascade of defences within stem cells themselves may cause more damage than good.
“It was thought cytokine storm happened due to the large influx of immune cells, but we can see it also happens in the lung stem cells themselves,” says cell biologist Purushothama Rao Tata from Duke University.
“Now we have a way to figure out how to energise the cells to fight against this deadly virus,” he adds.
In another set of experiments on the mini-lung, researchers found that administering low doses of interferons before infection slowed the spread of the virus, whereas reducing interferons before infection worsened the damage.
This suggests interferons are somehow mediating the immune response in our alveoli, slowing the cascade of cell death as the lung tries to get ahead of the infection.
But this may not be the whole picture; it’s just a small insight into what’s going on. Other recent studies show that while interferons might be a helpful treatment at certain stages of infection, at other times they can make matters worse.
While there are still many kinks and details that need to be ironed out in their model, researchers hope they can one day grow mini-lungs on which hundreds of experiments can be run at the same time, allowing us to figure out how the lung responds to infection and also how we can best protect it.
There’s never been a more important time to learn more.
The study was published in Cell Stem Cell.