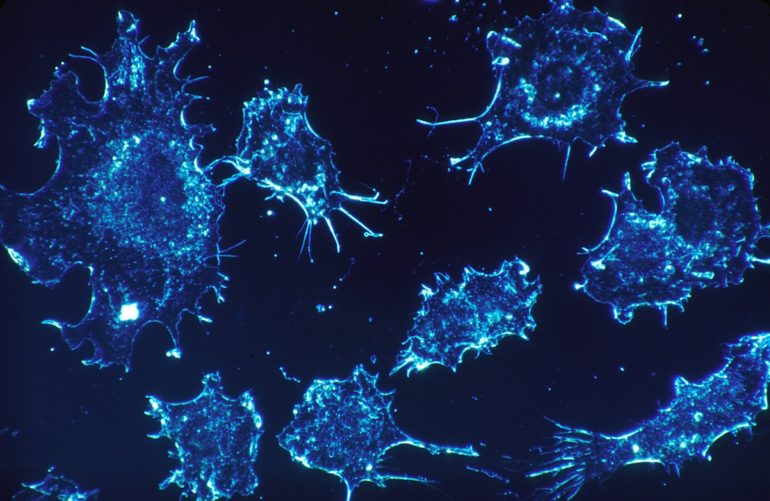
St. Jude Children’s Research Hospital scientists have identified factors that influence how children with acute lymphoblastic leukemia (ALL) respond to methotrexate. High-dose methotrexate is a part of modern curative therapy for ALL. The work provides insights to help optimize methotrexate treatment. The findings were published online today in the Journal of Clinical Investigation.
Using leukemia cell samples gathered through the Total 13 and Total 15 clinical trials for ALL, the researchers studied responses to methotrexate. The amount of active methotrexate found in the patients’ leukemia cells varied widely, which resulted in differences in how they responded to treatment.
“My lab tries to understand why we can cure 90% of children with ALL, but not the other 10%,” said corresponding author William Evans, PharmD, of St. Jude Pharmaceutical Sciences. “Getting enough chemotherapy inside tumor cells is necessary to produce the drugs’ intended effect, so we investigated what happens both inside and outside cells when we use methotrexate to treat cancer. What we’ve learned repeatedly is that every child is different.”
The researchers identified five factors that play a role in how much methotrexate gets inside leukemia cells. These are systemic clearance, treatment dosing, the ALL subtype, gene expression and the enzyme expressed by FPGS.
Systemic clearance, how the drug is removed from the bloodstream, was previously reported and confirmed by this study. Treatment dosing, giving the drug over 24 hours instead of four, allows much more drug to get inside the leukemia cells. This was also previously reported by St. Jude and confirmed by this study. Researchers also showed that the benefit of giving the drug over 24 hours holds true regardless of ALL subtype.
Analysis by subtype reveals important differences
Findings show that the ALL subtype makes a difference in response to methotrexate. T-ALL accumulates less of the drug and B-ALL accumulates more. The BCR-ABL-like ALL subtype (which is a relatively common kind of B-ALL) accumulates more methotrexate. This is important for physicians and pharmacists to know because BCR-ABL-like ALL is a high-risk subtype that needs more effective treatment. The finding suggests patients with BCR-ABL-like ALL could benefit from additional high-dose methotrexate in their treatment.
The team also looked at differences in the expression of specific genes in leukemia cells, particularly those encoding transporter proteins that control what crosses a cell’s membrane. SCL19A1 transports drugs into leukemia cells, and ABCC4 and ABCC1 transport drugs out. Children with the ability to import more of the methotrexate have better responses than children who have an excess ability to transport the drug out. Medications that inhibit these export pumps (like an ABCC4 inhibitor) could be tested as a way to improve responses to methotrexate in patients who over-express ABCC4.
The gene FPGS produces the enzyme that converts methotrexate to its active form inside cells. Certain subtypes of ALL (such as T-ALL) don’t express as much of the enzyme, which limits its ability to keep the drug inside the cells. Understanding how genetic differences among the ALL subtypes influence response to methotrexate may help physicians and pharmacists tailor treatment.
“Methotrexate remains an essential drug in the treatment of ALL,” said study author Ching-Hon Pui, M.D., chair of the St. Jude Oncology Department. “This study provides new insights into inter-patient differences in methotrexate polyglutamate accumulation, findings that can guide our use of this medication in future clinical trials to improve cure rates while reducing toxicities.”
New trial results question standard treatment plan for rheumatoid arthritis
More information:
Elixabet Lopez-Lopez et al. Pharmacogenomics of intracellular methotrexate polyglutamates in patients’ leukemia cells in vivo, Journal of Clinical Investigation (2020). DOI: 10.1172/JCI140797
Provided by
St. Jude Children’s Research Hospital
Citation:
Molecular mechanisms reveal how to make the most of methotrexate (2020, November 10)
retrieved 10 November 2020
from https://medicalxpress.com/news/2020-11-molecular-mechanisms-reveal-methotrexate.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.