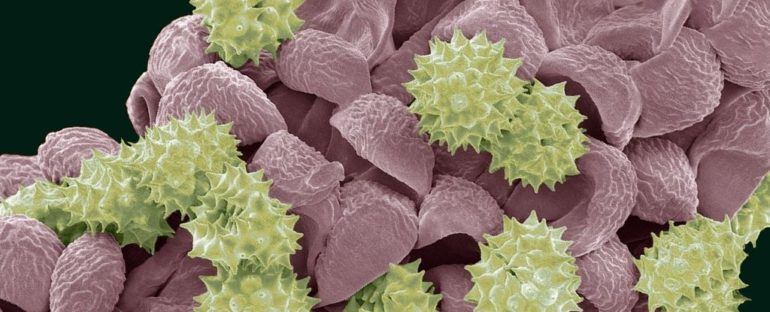
Those of us with hay fever are painfully familiar with the frustration caused by days of high pollen – the incessant leaking of eye and nose mucus, itchy ears, eyes and throat, bursting fits of sneezes, and sometimes headaches and asthma. Now, a new study suggests that in people with a chronic pelvic condition, high pollen could also be triggering bouts of pelvic pain.
More than 10 million people in the US live with the mysterious set of conditions known as urologic chronic pelvic pain syndrome (UCPPS) – a cluster of problems that include bladder pain syndrome and interstitial cystitis in women, chronic pelvic pain syndrome, and chronic prostatitis in men. They can cause debilitating symptoms like an urgent and frequent need to urinate, agony within the pelvic region, and painful sex.
Researchers have called UCPPS “one of the most frustrating urologic conditions to understand and manage” because its causes are still unknown as are its triggers of frustrating symptoms. A diagnosis of interstitial cystitis in women, for example, can involve bladder inflammation where all other possible known causes have been ruled out.
Everything from bacteria to psychological causes have been examined without much clarification.
However, case reports have suggested asthma and allergy medications can relieve UCPPS symptoms and patients have reported flare-ups coinciding with other allergies. So Washington University epidemiologist Siobhan Sutcliffe and colleagues decided to take a closer look at UCPPS’s link with a well-known allergen.
The team compared 290 patient’s flare-ups with pollen levels and found that while daily changes in pollen counts didn’t seem connected, when pollen rates exceeded a “medium” threshold symptoms flared up by 22 percent one or two days later.
“Our study provides evidence to suggest increased pollen counts may trigger symptom flares in people living with UCPPS,” said Sutcliffe.
The well-known process of mast cell activation in allergies that releases the histamines they carry is suspected to contribute to some of these UCPPS conditions. Animal studies have shown prolonged high levels of histamine in the bladder can make the bladder’s nerves hypersensitive. And histamines in urine appear to remain elevated for longer than in our blood as our bodies use this exit pathway to remove them.
The new research adds to this evidence and could help provide patients with some much-needed relief. But further research is needed to account for possible confounding factors that may have been missed, such as other environmental factors that might coincide with higher pollen levels or things like flower bouquets which could contribute to flares.
“Patients may benefit from taking antihistamines on days with high pollen levels, or from allergy testing and immunotherapy,” said Sutcliffe.
This study was published in The Journal of Urology.