Imagine going to the hospital for a bacterial ear infection and hearing your doctor say, “We’re out of options.” It may sound dramatic, but antibiotic resistance is pushing that scenario closer to becoming reality for an increasing number of people. In 2016, a woman from Nevada died from a bacterial infection that was resistant to all 26 antibiotics that were available in the United States at that time.
The U.S. alone sees more than 2.8 million antibiotic-resistant illnesses each year. Globally, antimicrobial resistance is linked to nearly 5 million deaths annually.
Bacteria naturally evolve in ways that can make the drugs meant to kill them less effective. However, when antibiotics are overused or used improperly in medicine or agriculture, these pressures accelerate the process of resistance.
As resistant bacteria spread, lifesaving treatments face new complications – common infections become harder to treat, and routine surgeries become riskier. Slowing these threats to modern medicine requires not only responsible antibiotic use and good hygiene, but also awareness of how everyday actions influence resistance.
Since the inception of antibiotics in 1910 with the introduction of Salvarsan, a synthetic drug used to treat syphilis, scientists have been sounding the alarm about resistance. As a microbiologist and biochemist who studies antimicrobial resistance, I see four major trends that will shape how we as a society will confront antibiotic resistance in the coming decade.
1. Faster diagnostics are the new front line
For decades, treating bacterial infections has involved a lot of educated guesswork. When a very sick patient arrives at the hospital and clinicians don’t yet know the exact bacteria causing the illness, they often start with a broad-spectrum antibiotic. These drugs kill many different types of bacteria at once, which can be lifesaving — but they also expose a wide range of other bacteria in the body to antibiotics. While some bacteria are killed, the ones that remain continue to multiply and spread resistance genes between different bacterial species. That unnecessary exposure gives harmless or unrelated bacteria a chance to adapt and develop resistance.
In contrast, narrow-spectrum antibiotics target only a small group of bacteria. Clinicians typically prefer these types of antibiotics because they treat the infection without disturbing bacteria that are not involved in the infection. However, it can take several days to identify the exact bacteria causing the infection. During that waiting period, clinicians often feel they have no choice but to start broad-spectrum treatment – especially if the patient is seriously ill.

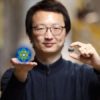
Amoxicillin is a commonly prescribed broad-spectrum antibiotic.
TEK IMAGE/Science Photo Library via Getty Images
But new technology may fast-track identification of bacterial pathogens, allowing medical tests to be conducted right where the…