Researchers at the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA are one step closer to developing stem cell therapies to regenerate skeletal muscle in humans. Working in mice, the UCLA team discovered how to make lab-grown muscle stem cells persist within muscle tissue and form new muscle.
Their study is published in the journal Nature Cell Biology.
Healthy adult muscle tissue has a powerful ability to repair itself, which explains why muscle soreness after a tough workout generally lasts no longer than a few days, and why pulled or strained muscles require little medical intervention to heal. But researchers have long struggled to give this same regenerative ability to lab-grown stem cells in order to develop treatments for people whose muscles cannot heal on their own—for example, in the case of diseases such as Duchenne muscular dystrophy, as well as in severe muscle injuries and age-related muscle loss.
For years, researchers have been trying to direct human pluripotent stem cells—which can become any cell type in the body—to generate skeletal muscle stem cells that can function appropriately in living muscle and regenerate muscle fibers. However, most of these studies have been confined to lab dishes. To gain a better understanding of these cells’ function and potential, the UCLA researchers transplanted them into the muscles of mice.
“This was an enormous effort involving functionally testing the human cells that have long been studied in a dish,” said April Pyle, UCLA professor of microbiology, immunology and molecular genetics and holder of the George and Nouhad Ayoub Centennial Chair in Life Sciences Innovation.
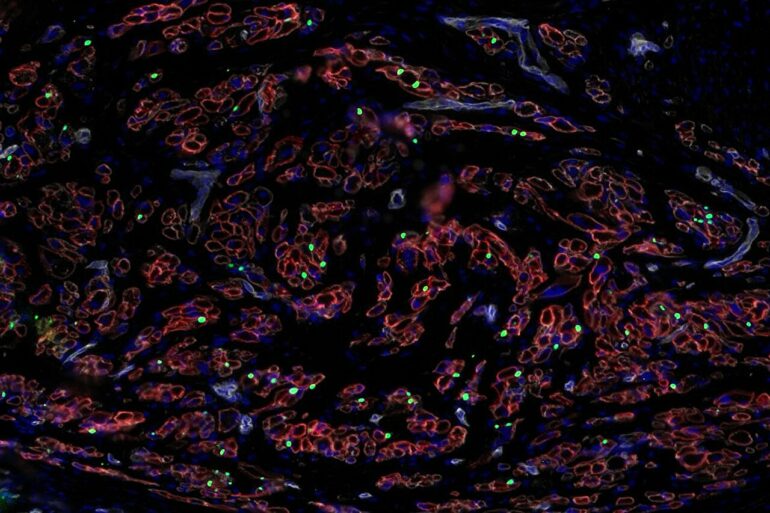
The cells’ survival, the scientists found, depends on complex molecular signals from the environment around them—called the stem cell “niche.” When the researchers created the optimal niche for lab-grown muscle stem cells, taking steps that included removing existing stem cells, the transplanted cells survived for more than four months and were able to repair muscle in successive injuries.
“We now know much more about how we can support muscle stem cells in their niche so they can direct muscle regeneration,” Pyle said.
In 2017, Pyle’s lab demonstrated how to generate muscle progenitor cells, the precursor to muscle stem cells, in a dish. More recently, she and her colleagues studied which genes were activated in different forms of muscle stem cells and muscle progenitor cells across human development and compared those to cells generated in a dish, shedding light on how the lab-grown cells might differ.
In the new work, the UCLA researchers moved to animal models, comparing how different muscle stem cells work when transplanted into the muscles of living mice. The researchers were surprised to find large differences between stem cells that had been grown in the lab and those isolated from healthy adult humans. The muscle progenitor cells that had been developed in the lab formed immature muscle cells that didn’t integrate efficiently, while adult muscle stem cells were better able to integrate into the mouse skeletal muscle niche.
“This is yet another example of how important it is to really rigorously test the functions of stem cells in living animals,” said Pyle.
To improve the ability of the stem cells to survive in adult muscle tissue, the researchers first removed the existing muscle stem cells of the mice—mimicking how patients receiving a bone-marrow transplant first have their own bone marrow eradicated.
“There has been a long-standing thought in the stem cell world that new stem cells will do better when there aren’t other stem cells around to compete with,” said Pyle. “We wanted to test this in the muscle system for the first time.”
Not only did the transplanted muscle progenitor cells survive longer, but when the muscle became injured after the mice had received the new stem cells, it was able to repair itself using only the new stem cells.
“We’ve never seen this in any other context with muscle progenitor cells,” Pyle said.
When the team looked more closely at how the stem cells were taking root in the mouse muscles, they discovered that growing muscle fibers—the ones that had most recently regenerated—were critical in forming the optimal niche for stem cell survival. Further experiments also revealed which genes, when activated in stem cells, were critical to the stem cells persisting within muscle.
These findings suggest that in eventual stem cell therapies, researchers need to optimize both the muscle niche and the muscle progenitor cells themselves in order to ensure that transplanted stem cells survive.
“All these inroads into understanding how to support new stem cells within muscle tissue are going to be really important for developing these cells for future therapies for humans,” Pyle said.
Michael Hicks, an assistant professor at UC Irvine and a previous postdoctoral fellow and UCLA Broad Stem Cell Research Center trainee in the Pyle Lab at UCLA, is the first author and co-corresponding author of the study. Other UCLA authors include Kholoud Saleh, Devin Gibbs, Mandee Yang, Shahab Younesi, Lily Gane and Haibin Xi.
More information:
Michael R. Hicks et al, Regenerating human skeletal muscle forms an emerging niche in vivo to support PAX7 cells, Nature Cell Biology (2023). DOI: 10.1038/s41556-023-01271-0
Provided by
University of California, Los Angeles
Citation:
Stem cell research paves way toward regenerating skeletal muscle (2023, November 2)