Type 1 diabetes is fundamentally a disease of the immune system. At some point, for some reason, the body’s defenses destroy insulin-producing tissues in the pancreas, making it all but impossible to fine-tune the flow of glucose into cells.
Returning the pancreas to a state of functionality would give diabetics a new lease on life, yet for all the progress we’ve made in tissue-replacement, safely taming a traitorous immune system has been an insurmountable obstacle.
There are finally signs we might be able to clear that hurdle, with US researchers and engineers developing a nano-fiber implant that can shield a patient’s own insulin-producing cells from their immune system.
Early results are encouraging, with tests in mice demonstrating it could be an effective way to treat type 1 diabetes using actual pancreatic tissue, without the need for immunosuppressive drugs.
“The device, which is about the width of a few strands of hair, is micro-porous – with openings too small for other cells to squeeze into – so the insulin-secreting cells consequently can’t be destroyed by immune cells, which are larger than the openings,” says medical researcher Jeffrey R. Millman from Washington University.
(Wang et al., Sci Trans Med, 2021)
For nearly a century type 1 diabetes has been treated through timely injections of the glucose-mediating hormone insulin, a process that has undoubtedly saved countless lives.
Yet getting the perfect amount of insulin from a bottle into the body is neither comfortable nor risk-free. Getting the dosage wrong could mean a life-threatening medical emergency.
While modern digital technology has made amazing progress towards mirroring an authentic pancreas, we’re still a long way off matching biology’s ability to meter out the right amount of hormones right where they’re needed.
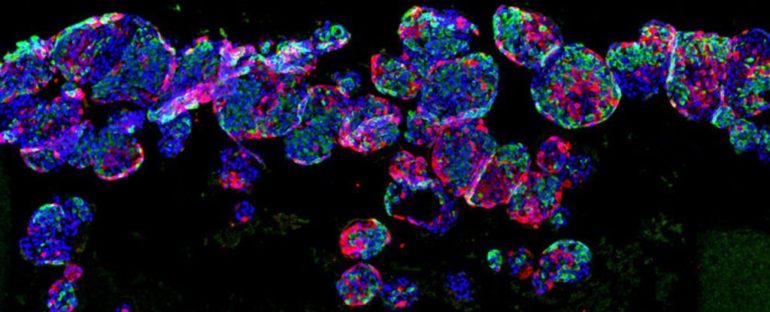
Advances in converting ‘blank’ stem cells into virtually any other cell in the body has allowed researchers to recreate a person’s insulin-secreting ‘islet’ tissues using little more than a sample of their own cells.
Making them is one thing – transplanting them into the body without attracting unwanted attention from the person’s own immune system is something else entirely.
“The problem is that in people with type 1 diabetes, the immune system attacks those insulin-secreting cells and destroys them,” says Millman.
“To deliver those cells as a therapy, we need devices to house cells that secrete insulin in response to blood sugar, while also protecting those cells from the immune response.”
Specially designed implants for shielding islet tissues from the ravages of the body’s immune system aren’t novel concepts. Some work better than others, reducing risks of scarring or providing oxygen or nutrients to extend the life of the implanted tissues.
One material with huge potential in encapsulating tissue implants is based on a polysaccharide found in the cell walls of algae, called alginate.
Its ability to avoid triggering an immune response itself makes it a suitable candidate. The challenge for researchers was to turn it into a capsule that could be removed periodically to replace the exhausted pancreatic tissue inside.
This led to the development of TRAFFIC – a thread-reinforced alginate fiber for islet encapsulation. If not for the fact the alginate is prone to swelling and breaking over time, it might have been a winning solution.
Millman and his team have now improved on TRAFFIC by weaving a medical-grade thermoplastic around an alginate hydrogel core, giving it the right mix of stealth, robustness, and porosity.
Tested in diabetic mice, the ‘nanofiber-integrated cell encapsulation’ (NICE) device helped the animals maintain their glucose levels for up to 200 days using human islet cells. The devices also scaled up well for implanting and retrieval in dogs.
It’s promising progress, though solutions such as these can’t come soon enough for the roughly one in every 7,000 people with a type 1 diabetes diagnosis.
“The device we used in these experiments protected the implanted cells from the mice’s immune systems, and we believe similar devices could work the same way in people with insulin-dependent diabetes,” says Millman.
This research was published in Science Translational Medicine.