Masks to protect people from illness come in all shapes and sizes, unfortunately.
During the early stages of the COVID-19 pandemic, a team at Rice University’s George R. Brown School of Engineering and the University of Texas MD Anderson Cancer Center went looking for and found a way to make standard surgical masks better at keeping out small airborne droplets that might contain the SARS-CoV-2 virus.
They came up with an easily manufactured adhesive silicone harness that allows light surgical masks to match and sometimes exceed the federal safety standards for N95 and KN95 masks.
A study led by Jeannette Ingabire, a Systems, Synthetic and Physical Biology graduate student in the Rice lab of electrical and computer engineer Jacob Robinson, appears in JAMA Network Open, part of the American Medical Association group of journals.
The team won a small grant in the first round of awards from Rice’s COVID-19 Research Fund to make surgical masks better suited to the crisis. “N95s were hard to get at the time, so it seemed logical to improve the flimsy surgical masks you see in hospitals,” Robinson said. “Now, of course, good masks are easier to get, but you never know when our solution will be needed.”
The project began when co-author Dr. Sahil Kapur, an assistant professor in the Department of Plastic Surgery at MD Anderson, approached Rice engineers with an idea for a harness to make surgical masks fit more snuggly around the face.
Based on Kapur’s concept, Rice’s Caleb Kemere, an associate professor of electrical and computer engineering and of bioengineering, designed several concepts, tried them on himself and determined they could be laser-cut from a single sheet of elastomer.
Ingabire and the Rice team 3D-printed mannequin heads of different shapes and sizes as specified by federal regulations. Once they assured proper fit with the mannequins, Ingabire and Hannah McKenney, a Rice alumna now at MD Anderson, recruited more than three dozen COVID-negative volunteers from among “essential personnel” at the institutions to judge the masks for comfort and sit for airflow tests with an infrared camera.
The camera quickly revealed where air was leaking in and out of ill-fitting masks—most often near the nose and eyes—leading to a revision of the harness.
The team’s version 2.1 closed the gaps for most wearers by widening the harness along the slope of the nose while reducing the amount of material overall to preserve the wearer’s field of view. The rubbery harnesses give the mask more of the form of an N95, with better sealing than the surgical mask alone.
“That was a suggestion from clinicians at MD Anderson who told us if something is really big, it can interfere with a surgeon’s eyesight,” Ingabire said. “So the final version fits more snugly around your nose. If you want people to use something for a long time, it has to be comfortable.”
The revised harness/mask combo easily passed a “filtering facepiece respirator” evaluation that proved it to be 15 times better at stopping droplets than surgical masks alone. Though the masks themselves are single-use, the harnesses can be removed, sanitized and used again, Ingabire said.
She said some of the volunteers were impressed enough to keep their harnesses.
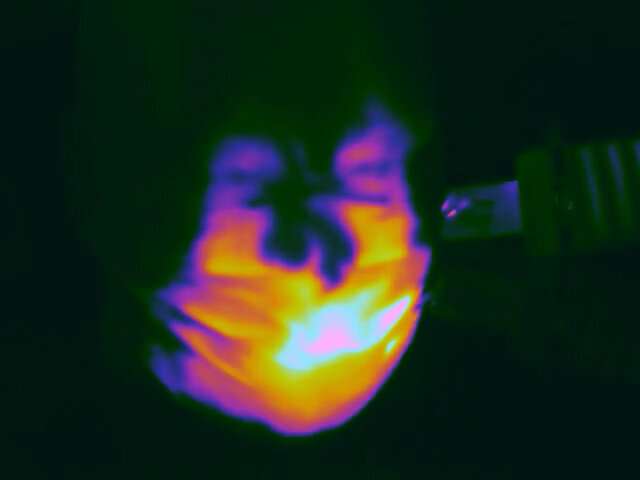
An infrared image shows hot air supplied to a mannequin by a hair dryer leaking from around the nose and on the side of a standard surgical mask. Rice University engineers designed a silicone harness that stopped the leaks. © Robinson Lab/Rice University
“A few grabbed some,” she laughed. “When they saw they passed the same fit test they use to evaluate an N95 in a hospital, they said, ‘Can I have this?'”
Co-authors of the paper include Rice alumnus Krishna Badhiwala and postdoctoral researcher Charles Sebesta. Robinson is an associate professor of electrical and computer engineering and of bioengineering.
More information:
Jeannette Ingabire et al, Evaluation of Aerosol Particle Leak and Standard Surgical Mask Fit With 3 Elastomeric Harness Designs, JAMA Network Open (2022). DOI: 10.1001/jamanetworkopen.2021.45811
Citation:
Research team’s mask adaptation strategy helps surgical masks to meet same standards as N95 and KN95 masks (2022, February 7)



