Although a vaccine could be the ultimate solution to curb the COVID-19 pandemic and stop future ones, it will not be 100% effective. If it is anything like the flu vaccine, it will most likely be slightly more than 50% effective.
What is important to recognize is that a vaccine can protect but cannot treat an already infected person. In contrast, drugs including laboratory-made antibodies (Y-shaped proteins that can help fight a foreign substance) can do both – protect and treat. This is why currently many companies are developing antibodies for prevention and therapy of COVID-19. Physicians would inject patients with these antibodies, which would immediately recognize and inactivate the virus. Such a therapy would bridge the lag until the patient’s immune system was able to produce enough of its own antibodies; some patients with weak immune system may never produce antibodies to fight the virus.
I am an antibody engineer and infectious-disease scientist interested in using the smallest part of the antibody – called a domain – as therapeutics for emerging viruses, including SARS-CoV-2. Domains combine some advantages of small molecule drugs and large standard antibody molecules. My colleagues and I have now engineered such an antibody-like molecule that both blocks and treats SARS-CoV-2 infection in animals studies and is now a promising drug candidate for human trials. This research has been published in the journal Cell.
Antibodies as drugs versus small molecules as drugs
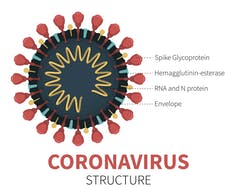
An antibody works by recognizing and binding to the disease-causing virus. When the antibody attaches to the spike protein of SARS-CoV-2, the spike is blocked from its lock-and-key interaction with the ACE2 protein on human cells. My colleagues and I are trying to develop drug molecules that mimic a body’s natural antibody response, blocking the spike protein from infecting the cell, replicating and causing disease.
Small drug molecules can penetrate tissue very well and can be administered conveniently as pills. However, because of the size, these small molecules are not highly specific and can bind to many human proteins and cause side effects.
Large biological drug molecules, including naturally occurring antibodies, by contrast, do not penetrate tissue very well. Antibody treatments must also be administered intravenously in a doctor’s office. The advantage is that antibodies are highly specific. They do not interfere with other human proteins and rarely cause side effects.
The challenge is combining the specificity of large native antibodies with those of small-molecule drugs that can penetrate tissues. An approach that my colleagues and I are testing is to take the domain, which is responsible for specifically binding to the target, like a virus, and just use this part of the antibody as a drug to block the spike protein of the virus from infecting cells.
How do we discover new antibody therapeutics?
Viktoriia Ilina/iStock/Getty Images Plus
At the University of Pittsburgh Center for Antibody Therapeutics, we developed a methodology that allowed us to discover stable human antibody domains that can bind with great strength and specificity to other molecules, including viral proteins.
The first step was to identify antibody genes from many humans, then separate those that encode just the antibody domains of interest – so-called “variable domains.” Then my colleagues and I created a collection containing more than 100 billion antibody domains with different specificity. This means that we have instructions for more than 100 billion little antibody fragments, one of which we hoped would bind tightly to the spike protein of the coronavirus.
By using a process called panning (as in the Western movies where gold hunters use pans to separate gold particles from sand), in just one week we separated the weak-binding or nonbinding domains from those that bound to the target – in this case the SARS-CoV-2 spike protein.
[The Conversation’s newsletter explains what’s going on with the coronavirus pandemic. Subscribe now.]
Finding and testing antibody domains to treat COVID-19
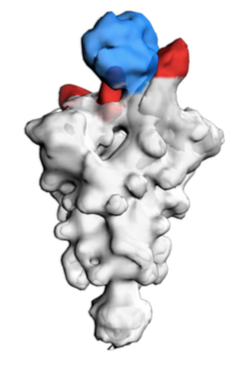
Li W et al. Cell 2020, CC BY-SA
By using as bait a small portion of the SARS-CoV-2 spike protein – called the receptor binding domain, which is key for binding to and infecting human cells – we “fished” in our very large collection of antibody domains and identified one that we call ab8, which binds strongly and specifically to the spike protein.
To increase the binding strength of ab8 and ensure it stays in the blood for a long time, we added a fragment of the antibody called Fc. This increased the size of the molecule but still it was smaller than the full-size antibody.
An antibody has a better chance of penetrating tissue the smaller it is. An antibody domain, which is about one-tenth the size of an antibody, is able to penetrate tissues and access areas where a virus is doing significant damage, like the lung.
Before we could determine whether ab8 was an effective drug we had to test it against live SARS-CoV-2 virus in living animals. Such experiments can only be done in special facilities called Biosafety Level 3 laboratories.
Taking ab8 from the lab to life
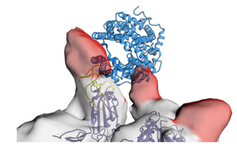
Li W et al. Cell 2020, CC BY-SA
Ultimately I hope that this tiny ab8 antibody domain could be mass-produced and then injected into people to either prevent infection – by binding to a spike protein of an invading coronavirus before it infected a human cell – or to reduce the severity of COVID-19 once they were sick.
Our collaborators at the University of Texas Medical Branch in Galveston were the first to show that ab8 was exceptionally powerful at neutralizing SARS-CoV-2 when tested on infected cells in the laboratory.
Our collaborators at the University of North Carolina confirmed these results and then showed that even tiny quantities of ab8 – as little as 50 micrograms per mouse – dramatically reduced the virus tenfold. (One microgram is one-millionth of a gram.) And, at higher doses, the virus was completely blocked from infecting cells.
Our colleagues at the University of Saskatchewan tested ab8 in larger animals: hamsters. They infected the hamsters with SARS-CoV-2 and then administered the drug. Ab8 reduced the virus in the hamsters dramatically.
Finally, our collaborators at the University of British Columbia used sophisticated electron microscope-based methods to visualize and understand how exactly ab8 neutralizes and blocks the virus. The images revealed that it does so by binding to exactly the same location on the viral spike protein used to attach to and gain entry into a human cell. This means that ab8 is functioning as a decoy receptor.
I cannot emphasize enough the collaborative nature of this research that led to the discovery of the therapeutic and preventive properties of ab8, which suggested that the molecule could also be highly effective and safe in humans.