Over the last 15 years, many African nations have made major strides towards enabling millions of HIV-positive people to access HIV antiretroviral therapy. This has helped to treat individual patients and maximize their health, as well as help lower the risk for transmission of HIV to others. But the lack of a key lab test needed to track whether HIV therapy is working optimally—known as HIV viral load testing—has been an obstacle to optimal patient care.
Now, a team of scientists at UC San Francisco and Makerere University in Kampala, Uganda have developed and tested an intervention that makes use of a portable laboratory testing technology to help HIV providers order, process, and receive HIV viral load results quickly, and shorten the time it takes for patients to get their results.
By using a hub-and-spoke system to create regional testing hubs serving local clinics, instead of centralizing viral load testing in the capital city, scientists were able to reduce the time it takes to get results from about two months to just one day.
Importantly, the study found a significant increase in viral suppression among the patients served by the hub-and-spoke clinics, the goal of making viral load testing more timely and more widely available. One year after the intervention, viral suppression was 83.1 percent in the intervention clinics and 76.0 percent in the control clinics.
Faster turnaround improves care
Time is of the essence in HIV care, and viral load measurements are a crucial tool in knowing whether treatment is working. This is especially true for higher risk patients, including pregnant women, and patients whose viral load results are already detectable.
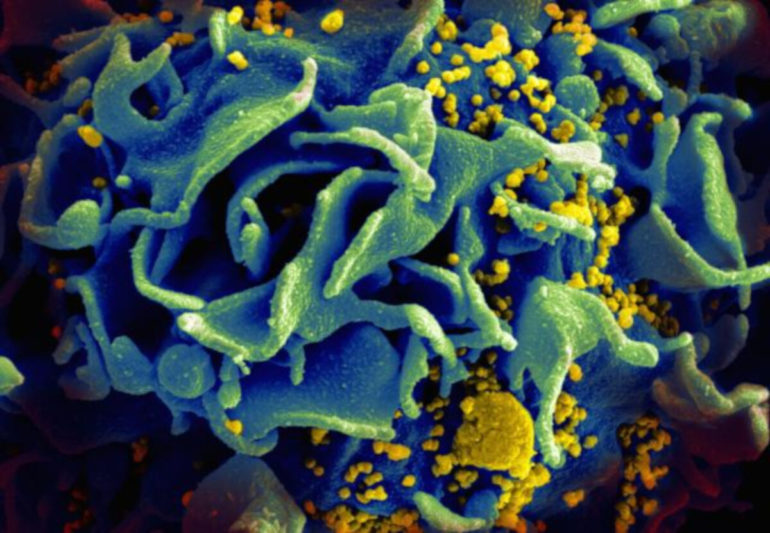
When the virus is undetectable in blood, doctors know that patients are taking their medicine and that the drugs are effectively fighting the virus. That protects the patient from inflammation and other ill effects of the virus, and it also prevents someone from spreading it to other people.
But when a patient has a detectable viral load, it can indicate that the person is not getting their medicine or that they have a resistant strain of the virus.
“If those problems are occurring, you want to detect them as soon as possible,” said Vivek Jain, MD, MS, associate professor of medicine at UCSF in the Division of HIV, Infectious Diseases and Global Medicine at Zuckerberg San Francisco General Hospital, and co-principal investigator of the study. “The best way to do that is with HIV viral load testing that gives you the results quickly.”
The RAPID-VL study included 2,400 people and was conducted in prototypic, rural Ugandan HIV care clinics run by the Ministry of Health. Jain presented the results Monday at the International AIDS Society 2021 global conference, which was held virtually.
Decentralizing testing infrastructure
One of the biggest challenges to delivering timely HIV care and viral load monitoring in rural Uganda, where the study was conducted, is that patients attend clinics in rural areas and rely on a system that transports blood samples to the capitol city, Kampala, where the national viral load testing infrastructure is centered. The capitol has a large and well-developed laboratory complex with sophisticated machinery, and it conducted more than 1.25 million viral load tests a year in 2019 and 2020. But it can take weeks or months for those results to filter back to the clinics and be delivered to patients.
The UCSF and Makerere scientists reasoned the viral load tests could be done much more quickly but still accurately on small, portable machines (the Cepheid Xpert VL platform) located closer to the clinics. So, they created two viral load testing hubs, each with an Xpert machine, and each serving 10 local clinics. The aim was to do the viral load tests and convey the results within a day.
And it worked. Turnaround times were reduced from a median of 56 days for the clinics that were still being served by the central testing laboratory in Kampala to just one day for the clinics served by the new regional testing hubs.
“The hope was to decentralize viral load testing to help speed up results, and make it possible to take faster clinical actions,” Jain said. “All of the testing equipment doesn’t have to be in this one major laboratory in the capital city. You could imagine a couple hundred small hubs that get dispersed around the country. It allows for a much faster loop to get your results.”
The success of the trial support the new conditional recommendation by the World Health Organization to offer viral load testing at or near the point of care to monitor HIV treatment.
“Patients in the clinics and the clinicians working with them reported good experiences with the rapid viral load testing system, noting it was feasible, useful, and improved overall care,” Jain said.
How innovation can help end the AIDS epidemic by 2030
More information:
V. Jain et al, RAPID-VL intervention improves viral load ordering, results turnaround time and viral suppression: a cluster randomized trial in HIV clinics in Uganda, https://srv2.key4events.com/key4register/AbstractList.aspx?e=71&preview=1&aig=-1&ai=4975
Provided by
University of California, San Francisco
Citation:
Faster test results mean better outcomes for HIV patients (2021, July 26)
retrieved 26 July 2021
from https://medicalxpress.com/news/2021-07-faster-results-outcomes-hiv-patients.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.