The job description for a red blood cell isn’t considered to be overly complicated. Pick up oxygen, drop off oxygen. Wash, rinse, repeat. But when it comes to protecting the body against infection, it’s their white cell sisters that we’ve been giving all the credit to.
However, a new study led by researchers from the University of Pennsylvania in the US has confirmed red blood cells also play a critical role in inflammation, one that could make a life-or-death difference.
As far back as the middle of last century scientists had their suspicions that red cells played some kind of role in keeping invaders at bay. By the 1990s, researchers were uncovering receptors on red blood cells that responded to inflammatory messenger chemicals called cytokines.
It all pointed to something afoot. Meanwhile, there was also the inexplicable loss of blood cells – anemia – that often comes with sepsis.
“Acute inflammatory anemia is often seen early after an infection such as parasitic infections that cause malaria,” says pulmonologist Nilam Mangalmurti, the senior author on the recent investigation.
“For a long time we haven’t known why people, when they are critically ill from sepsis, trauma, COVID-19, a bacterial infection, or parasite infection, develop an acute anemia.”
Just a few years ago Mangalmurti and her team showed how red blood cells could scavenge the free-floating scraps of mitochondrial DNA that spilled from injured tissues, triggering a response that helps regulate inflammatory responses in the lungs.
But missing pieces of the puzzle remained. How does a fragment of DNA from our own body turn an oxygen-carrying cell into an infection-fighting machine? And why do they disappear?
A major key could be found in the protein that grabs onto the DNA. Called toll-like receptors (TLR), they’re normally found on sentinels like the microbe-munching macrophages, where they respond to the short sequences as a sign that the body is under invasion.
Initial tests on human and chimpanzee blood confirmed they also existed on red blood cells. Thanks to their recent analysis of blood samples taken from sepsis and COVID-19 patients, the researchers now know that the number of receptors, specifically TLR9, increases during infections.
The TLR9 receptor readily mops up the released pieces of DNA, some of which contain sequences that bear an uncanny resemblance to those in many virus and bacterial segments of nucleic acid.
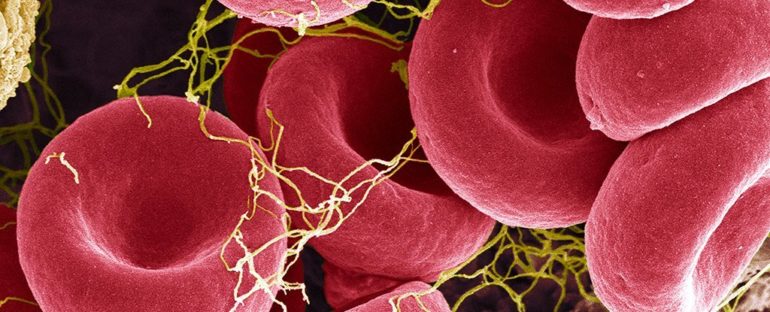
Under carefully managed laboratory conditions, these DNA-triggered red blood cells looked shockingly abnormal: Their typically concave ‘donut’ shape was warped.
This change in morphology is a check-box for sepsis, so seeing it so obvious under these lab conditions was a clear sign that the team was on the right path.
In no time, the malformed red blood cells began to disappear, swallowed up by macrophages. The engulfing in turn set off a chain reaction of inflammatory messengers that would effectively sound the alarm for the immune system to act in haste.
Tests carried out on mice infected with parasites backed up what they were seeing outside of the body. Sure enough, mitochondrial DNA was elevated on the mice’s red cells, compared with those from non-infected animals.
Triggering inflammation in parts of the body that otherwise aren’t in any danger of infection can be bad news, especially in people with autoimmune disorders. So finding ways to prevent red blood cells from overreacting to the presence of free-floating mitochondrial DNA would be immensely helpful.
It would also save lives for those at risk of acute anemia.
“Right now when patients in the ICU [intensive care unit] become anemic, which is almost all of our critically ill patients, the standard is to give them blood transfusions, which has long been known to be accompanied by a host of issues including acute lung injury and increased risk of death,” says Mangalmurti.
“Now that we know more about the mechanism of anemia, it allows us to look at new therapies for treating acute inflammatory anemia without transfusions, such as blocking TLR9 on the red blood cells.”
This research was published in Science Translational Medicine.