Researchers at the University of York are a step closer to identifying ways to support clinicians in predicting drug treatment outcomes for patients with visceral leishmaniasis in Brazil.
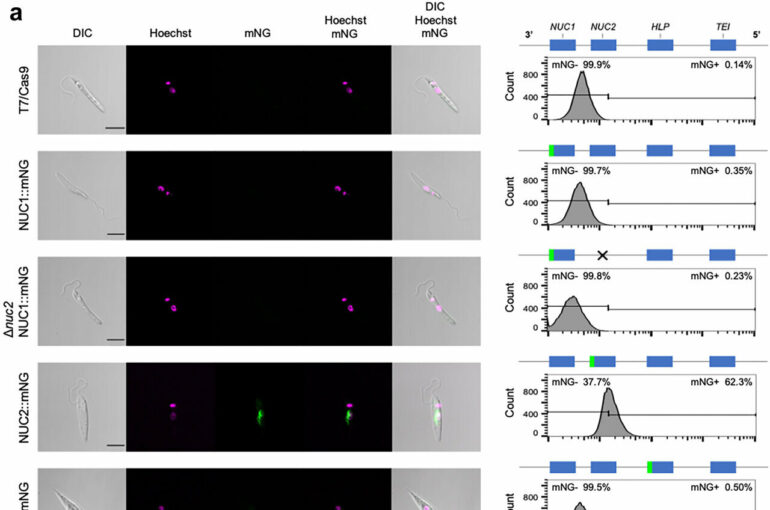
Scientists at York had previously shown that the absence of four particular genes in some strains of Leishmania infantum parasite found in Brazil makes it less susceptible to an oral drug called miltefosine.
The absence of these genes correlates with resistance to the drug, which means that Brazilian patients would benefit from a prognostic test, but in order to do this scientists first had to identify what it was about the gene that made the parasite drug-resistant.
During a clinical trial using miltefosine treatment, 40% of patients relapsed within six months, but the presence of the genes in the parasite found in India, however, meant that after a month of treatment, the disease could be cured with a lower risk of relapse.
As a result of its “failure” in Brazil, the medication is not licensed in the country and therefore there is very little that can be done to manage the disease in patients, other than intravenous drugs which can prove to be a burden on medical facilities who have to deliver it.
The team, in collaboration with colleagues from the Universidade Federal do Piauí and and the Universidade Federal do Espírito Santo, have now taken the work a step further and identified the enzymes that make the difference between treatment success and failure.
Juliana Brambilla Carnielli, Research Associate at the University of York’s Department of Biology, said, “Now that we have narrowed the search from a set of genes to an enzyme, the potential for developing a blood test that can accurately predict patient outcome is more likely.”
“There is no one-size-fits all treatment, and so a personalized medicines approach is needed, whereby a prognostic test to predict treatment success at an individual level can be provided.”
“This disease impacts people in India, Brazil, Africa and some parts of Europe, so it really is important that we understand more about how the parasite lives in humans and reacts to drugs.”
Leishmaniasis is a parasitic disease transmitted to humans by the bite of the infected female sandfly. With 50,000 to 90,000 new cases worldwide each year, it causes fever, substantial weight loss, swelling of the spleen and liver and anemia and can be fatal if left untreated.
The parasite first arrived in South America from Europe in the 1600s and has changed and adapted over time. Jeremy Mottram, Professor of Pathogen Biology and Director of the York Biomedical Research Institute, said, “This latest finding means that we are much closer to moving to clinical trials on patients in Brazil and to understand whether prognostic tests early in the disease progression and tailored medicines could reduce the numbers of patients relapsing with the disease.”
Up to 2,500 patients presented with the condition in Brazil in 2019 with a lethality rate of 9%, the highest recorded over the last 10 years, creating a significant burden on hospital resources.
The work is published in the journal eBioMedicine.
More information:
Juliana B.T. Carnielli et al, 3′Nucleotidase/nuclease is required for Leishmania infantum clinical isolate susceptibility to miltefosine, eBioMedicine (2022). DOI: 10.1016/j.ebiom.2022.104378
Provided by
University of York
Citation:
One step closer to tackling drug resistant parasites in Brazil (2022, December 1)